Clinical Research 101: How to Perfect Your Study Start-Up Process
It is in the study start up that the success of any clinical trial is demonstrated. Clinical research start up is vital as it establishes the framework of the trial from the development of the protocol to regulatory approval and site recruitment. For clinical research teams, it is important to understand how the study start up process works and how it ensures the continuity of the trial and its compliance with the set regulations.
In this comprehensive guide, we will explore the various components of study start-up in clinical research and the steps that can be taken to perfect this important phase. If you are new to clinical trials or a seasoned researcher, this article will aid you in refining your approach and skipping some common pitfalls. We will also discuss the role of regulatory requirements, budget planning, site activation and investigator selection.
What is Study Start-Up in Clinical Research?
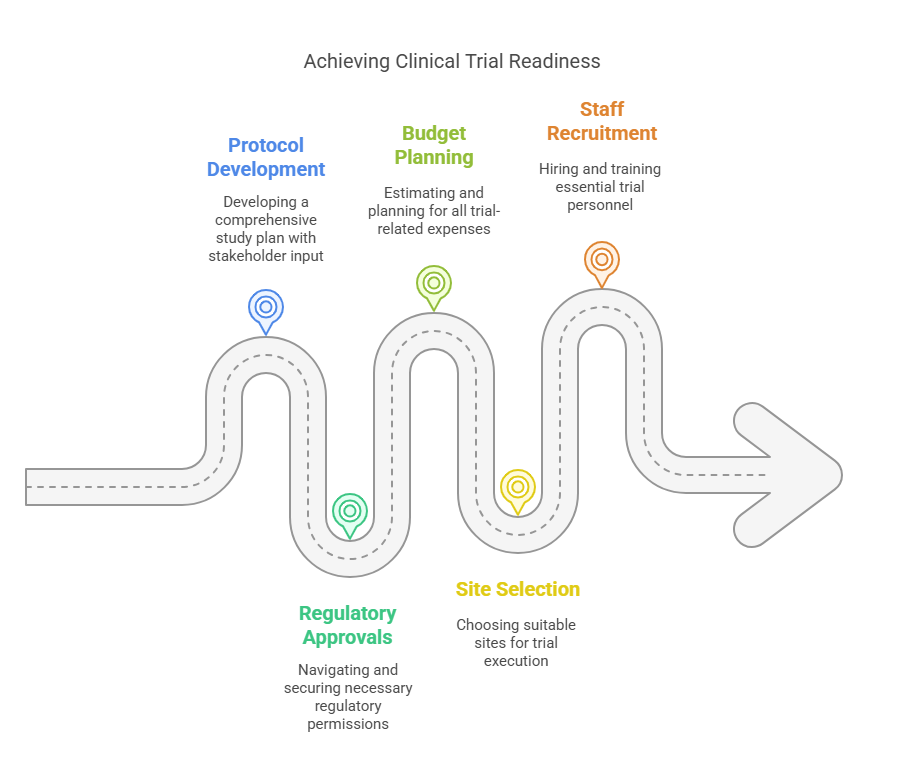
Study start-up is the initial phase of a clinical trial that involves the preparation, planning, and implementation of all necessary tasks to initiate a clinical trial. This process typically includes:
Study design and protocol development,
Regulatory submissions and approvals,
Budget planning and contract negotiations,
Site identification, selection, and activation,
Investigator and staff recruitment.
The aim of study start-up is to make sure that all the practical, legal, and organizational aspects are ready for when patient enrollment is to begin. Effective start-up reduces time lost, guarantees that the study conforms to the necessary rules, and facilitates the development of a good working relationship between the researchers and other interest groups.
Key Components of the Study Start-Up Process
Perfecting your study start-up process requires a thorough understanding of the key components involved in this phase. Below are the essential elements of study start-up in clinical research:
1. Protocol Development and Design
The protocol is the reference of what your clinical trial should look like. It explains the purpose of the study, how data will be collected, who is eligible to participate, what treatments will be given, and how it will be done. A good protocol is important to make sure that your study is scientifically appropriate and morally acceptable.
In developing the protocol however, it is very important that key stakeholders such as investigators, sponsors and regulatory authorities are involved in order to ensure that the study is consistent with the required guidelines and objectives. Moreover, the protocol has to be versatile enough that any modifications or amendments that are required during the course of the trial can easily be factored in.
2. Regulatory Submissions and Approvals
One of the biggest challenges of clinical research is navigating the regulatory landscape. Clinical trials are highly regulated by regulatory authorities like the FDA, EMA, and others, with very specific guidelines that are not adhered to can result in significant delays, or even the termination of the trial.
During the start-up phase, it’s important to submit all necessary documentation to the relevant regulatory agencies. These submissions typically include:
Investigational New Drug (IND) application,
Institutional Review Board (IRB) approvals,
Ethics Committee approvals,
Informed consent forms.
Adherence to Good Clinical Practice (GCP) guidelines is therefore vital at this stage of the process. The start up process would be accelerated by efficient regulatory submissions and approvals, so your study can start without having to wait for unnecessary delays.
3. Budget Planning and Contract Negotiations
Before initiating a clinical trial, it is essential to develop a comprehensive budget that accounts for all costs related to the study. Budget planning should cover expenses such as:
Investigator fees,
Site costs,
Patient recruitment,
Regulatory submissions,
Data management and monitoring.
It is very important to have accurate budget planning to avoid unforeseen expenses that can exit at the end of the trial and put a strain on the resources. Furthermore, negotiations of contract with sites and vendors should take place during the start up phase to ensure that there is a clear understanding of the roles, responsibilities and payment terms of the parties involved.
4. Site Selection and Activation
Selecting appropriate clinical trial sites is important for the effectiveness of your study. These factors include; previous collaboration with other similar trials, ability to recruit patients, infrastructure, and qualifications of the staff. Moreover, sites should be able to facilitate data collection and patient monitoring through the required equipment and technology.
Site activation implies checking that all the necessary clearances have been obtained, all the contracts are signed, and the study personnel have been instructed on the protocol. A good site activation process ensures that the sites are prepared to receive patients when the recruitment starts.
5. Investigator and Staff Recruitment
Another crucial aspect of study start-up is the recruitment of properly trained investigators and research staff. Investigators are key to making sure that the trial is conducted properly, following the protocol and the regulatory standards. This is why it is important to select investigators with the right expertise and experience.
Along with investigators, other essential staff like clinical research coordinators, data managers and study nurses must also be hired and trained during the start up phase. This guarantees that the team is ready to go once patient recruitment does start.
Best Practices for Optimizing the Study Start-Up Process
Streamlining the study start-up process is essential for minimizing delays and ensuring the timely initiation of clinical trials. Below are some best practices that can help you perfect your study start-up process:
1. Create a Detailed Study Start-Up Plan
Having a good plan is essential to the success of a study start-up. The plan should include; the important milestones, the time lines and the activities that must be accomplished before the patient recruitment can commence. It includes such as regulatory submissions, site selection, budget approval, and training of staff.
2. Implement a Study Start-Up Checklist
Using a checklist can help ensure that no important tasks are overlooked during the start-up phase. A study start-up checklist should include items such as:
Finalizing the protocol,
Submitting regulatory documents,
Negotiating contracts,
Activating sites,
Training staff.
3. Maintain Open Communication with Stakeholders
It is essential to have effective communication during the start-up phase of a clinical trial. The sponsors, investigators, regulatory authorities, and site staff must be informed of the progress of the trial and any issues that may happen. It can be helpful to have regular meetings and status updates to make sure everyone is in sync with where the study is, and where it is hoping to be.
4. Leverage Technology
Using digital tools like CTMS (Clinical Trial Management Systems) and other tools can also help to streamline the study start-up process; for instance, document submission, budget tracking, and site activation can be made more efficient through automation. Implementing technology may reduce the time and energy investing in the management of the start-up phase and thus enhance the overall efficiency.
5. Anticipate and Mitigate Risks
Such as regulatory delays and site activation issues, potential risks can delay and happen in clinical trials, but they can be reduced through proactive risk management. Site activation issues, regulatory delays and other such factors are potential risks that need to be considered during the start up phase of the trial and what should be done in case they occur. Thus the implementation of this approach will assist in the trial’s progress not to be derailed even in the event of unexpected obstacles.
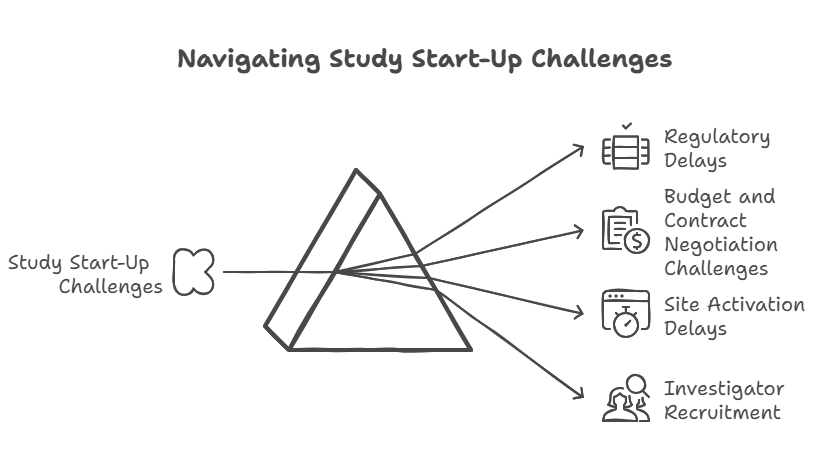
Common Challenges in Study Start-Up
The study start-up process can be fraught with challenges that can delay the initiation of clinical trials. Below are some common challenges and strategies for overcoming them:
1. Regulatory Delays
A delay in obtaining regulatory approvals is one of the most common problems in study start up. To avoid this it is necessary to include all the necessary documents and to communicate with regulatory agencies frequently to find out where your submissions stand.
2. Budget and Contract Negotiation Challenges
Negotiating contracts and budgets can be time consuming, especially when there are multiple sites or vendors. To expedite this process it is important to have a clear understanding of the study’s financial requirements and to work closely with legal and financial teams to finalize agreements quickly.
3. Site Activation Delays
If sites are not properly prepared or if they lack the necessary regulatory approvals, site activation can be delayed. This can be prevented by keeping regular contact with sites and giving them all documentation and training that they may need in advance.
4. Investigator Recruitment
A problem of finding suitable investigators with the needed skills and free schedule is a rather real one. In order to solve this issue it is required to start the recruitment process at an early stage and to use the professional relationships and contacts within the industry in order to find the list of possible investigators.
Perfecting Your Study Start-Up Process
It is very important to master the study start-up process for the success of any clinical trial. Clinical research teams can ensure that their trials are executed efficiently and with minimum delays by focusing on key components like protocol development, site activation, budget planning, regulatory submissions and investigator recruitment.
If you follow the best practices, use technology, and anticipate risks, you can optimize your study start-up process and set your clinical trial up for success. Not only will this benefit the trial itself, but it will also further medical knowledge and patient outcomes.
Conclusion
mastering the study start-up process is crucial for the success of clinical trials. By adhering to Good Clinical Practice guidelines, leveraging advanced technology, and implementing effective communication strategies, research teams can significantly enhance the efficiency of their start-up processes. Overcoming common challenges like regulatory delays and investigator recruitment requires proactive planning and collaboration. For those looking to deepen their understanding and skills in this area, the Clinical Research Coordinator Course offered by CCRPS provides valuable insights and training. Engaging with such educational resources can empower professionals to conduct more effective and compliant clinical trials.
Reference Links:
ClinicalTrials.gov - Study Start-Up Information
European Medicines Agency (EMA) - Clinical Trial Start-Up Requirements
World Health Organization (WHO) - Good Clinical Practice Guidelines
Stanford University - Clinical Research Study Start-Up Checklist
Relevant Course Links:
-
Key milestones in the study start-up phase include the completion of protocol development, obtaining regulatory and ethical approvals, budget finalization, site selection and activation, and the recruitment and training of investigators and staff. Each of these milestones is critical to ensure that the clinical trial is set up correctly and ready for patient recruitment.
-
The duration of the study start-up phase can vary widely depending on factors such as the complexity of the study, the number of sites involved, regulatory requirements, and the efficiency of the processes in place. Generally, this phase can take anywhere from a few months to over a year. Efficient planning and proactive management of potential issues can help reduce delays and shorten this timeframe.
-
Good Clinical Practice (GCP) guidelines are international quality standards that govern the design, conduct, performance, monitoring, auditing, recording, analysis, and reporting of clinical trials. They ensure that the data and reported results are credible and accurate, and that the rights, integrity, and confidentiality of trial subjects are protected. Compliance with GCP is mandatory in many countries for all studies that involve human participants.
-
Technology, particularly Clinical Trial Management Systems (CTMS), enhances the study start-up process by automating and streamlining various tasks such as document management, budget tracking, regulatory submissions, and site management. These technologies improve communication, reduce paperwork, and provide real-time monitoring, which helps in making quick adjustments and reduces the overall time spent on administrative tasks.
-
Strategies to overcome challenges in investigator recruitment include starting the recruitment process early, utilizing professional networks and industry contacts, engaging with investigator databases, and considering the use of social media platforms for wider outreach. Additionally, offering competitive study compensation and highlighting the scientific merit and potential impact of the study can attract qualified investigators.