Managing Clinical Research Teams: Leadership Strategies for PIs
Clinical trials succeed or fail not just on protocols—but on people management at the top. Principal Investigators (PIs) are the central operational force behind regulatory compliance, data integrity, and subject safety. But beyond GCP and protocol adherence, effective team leadership can determine the timeline, quality, and financial efficiency of an entire trial. This leadership burden requires more than seniority—it demands strategic capability, ethical backbone, and cross-functional orchestration under pressure.
As trials become increasingly global and complex, clinical research teams now involve 5–15 core roles across data, monitoring, patient care, and regulatory reporting. Miscommunication, misalignment, or burnout in even one function can cascade into critical protocol deviations or audit failures. PIs must therefore master not just delegation—but vision-setting, role clarity, and ethical stability. This guide breaks down how leading PIs build high-performance teams—and how to evaluate, course-correct, and evolve as a clinical leader across every trial phase.
Key Responsibilities of Clinical Research Leaders
A Principal Investigator (PI) is legally accountable for trial integrity, but the best clinical research leaders go far beyond minimal compliance. They translate protocols into action, rally multi-disciplinary staff under one goal, and uphold ethics even when under pressure from sponsors or CROs. Every PI must internalize and execute five core categories of responsibility.
1. Strategic Oversight of Protocol Execution
A strong PI maintains end-to-end oversight of protocol milestones. That includes:
Aligning trial operations with ICH-GCP and FDA 21 CFR requirements
Monitoring data integrity checkpoints and deviation trends
Reviewing trial progress in light of site-specific capacity, budgets, and enrollment goals
Even when tasks are delegated to sub-investigators or CRCs, the PI remains accountable for every major decision and deviation.
2. Building & Mentoring the Research Team
Research team structure isn’t static—it evolves with protocol complexity. PIs must:
Recruit or approve qualified CRCs, coordinators, and raters
Deliver SOP-based onboarding
Offer consistent GCP-aligned mentorship and performance feedback
The ability to develop internal talent pipelines directly impacts data quality and retention across trials.
3. Managing Compliance & Audit Readiness
PI leadership includes preparing for internal audits, IRB inspections, and sponsor reviews. This requires:
Ensuring source documentation aligns with CRFs
Creating defensible audit trails through timely signatures and logs
Rapidly addressing protocol violations or AE reporting lags
A PI who normalizes compliance culture reduces trial risk and accelerates close-out readiness.
4. Ethical Safeguarding of Trial Participants
This extends beyond informed consent. Leading PIs must:
Vigilantly monitor subject risk vs. benefit as new data emerges
Adjust enrollment strategies to ensure demographic equity
Act as patient advocates even when sponsor timelines are aggressive
They ensure ethics committees remain updated on all substantial protocol amendments or emergent risks.
5. Stakeholder Communication and Escalation
PIs act as the point of convergence between sponsors, CROs, IRBs, and internal teams. That includes:
Translating sponsor objectives into site-level tactics
Escalating red flags (e.g., serious adverse events, protocol drift) before they snowball
Leading DSMB conversations and site close-out meetings when necessary
Strong PIs don’t just manage—they mediate, clarify, and resolve.
Building & Managing High-Performance Clinical Teams
Clinical trial outcomes are directly tied to how well the research team performs under pressure. A PI's leadership must foster collaboration, reduce friction, and drive excellence across roles like CRCs, regulatory specialists, data managers, and sub-investigators. Here’s how the most effective clinical leaders consistently build high-performance teams from the ground up.
Define Clear Roles and Ownership from Day One
Ambiguity breeds conflict. Top-performing PIs begin by:
Mapping each trial function to a named individual or role (not just job titles)
Ensuring everyone understands primary, secondary, and shared responsibilities
Documenting handoff procedures between departments to avoid protocol gaps
When role clarity is embedded, accountability becomes part of the team’s culture.
Standardize Workflows Using SOPs and Playbooks
High-performing teams rely on repeatable systems, not ad-hoc fixes. PIs must lead:
Creation and implementation of site-specific SOPs for recruitment, AE reporting, data entry, and consent
Use of checklists and workflow playbooks tailored to protocol complexities
Continuous updates to documents as trial conditions evolve or scale
This avoids “oral tradition” problems and boosts inter-role reliability.
Establish Performance Metrics and Feedback Loops
Data isn't just for the sponsor—it's also for your team. Great PIs:
Set measurable KPIs for timelines, accuracy, protocol adherence, and retention
Conduct weekly or biweekly debriefs with transparent performance dashboards
Build constructive feedback sessions into team culture, not just annual reviews
When feedback is normalized, underperformance can be caught early and improved rapidly.
Prioritize Psychological Safety and Retention
Burnout and turnover sabotage long trials. Exceptional PIs address this by:
Allowing safe expression of workload issues or protocol concerns
Recognizing high-performers publicly and providing stretch roles where feasible
Monitoring emotional climate and preempting dysfunction through 1:1 check-ins
Retention rates correlate strongly with trial completion rates—keeping your team intact is mission-critical.
Invest in Ongoing Training and Cross-Functional Fluency
High-functioning teams know more than just their lane. PIs can:
Schedule cross-training sessions for overlapping functions (e.g., CRCs understanding regulatory logic)
Encourage GCP refreshers or certification upgrades through platforms like CCRPS Clinical Research Training
Invite external experts to audit or present on real-world case deviations
Cross-functional exposure minimizes tunnel vision and boosts adaptive resilience.
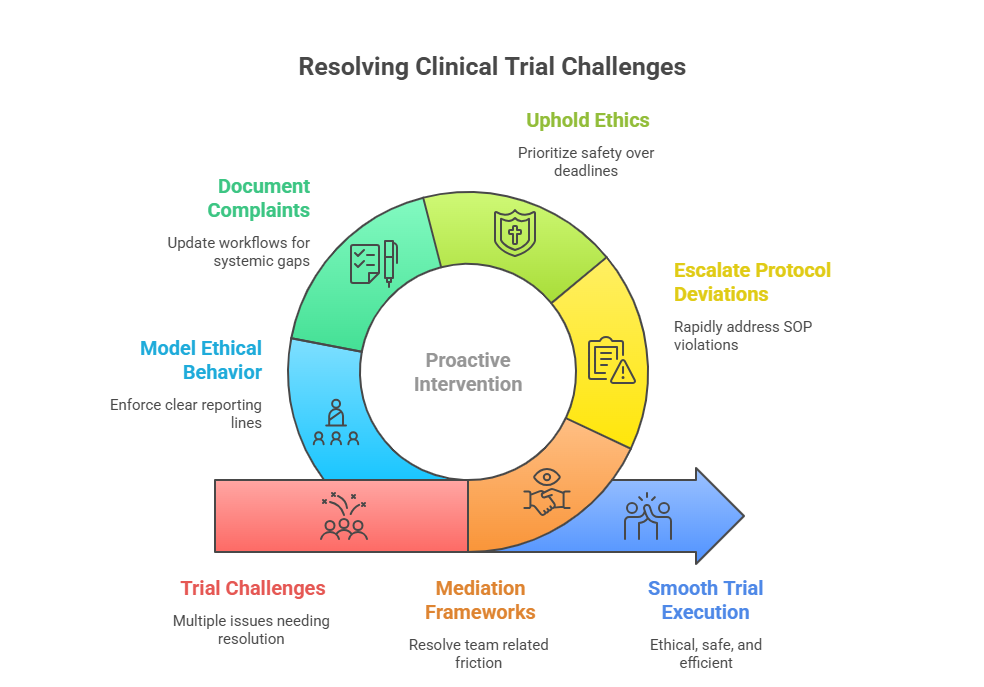
Conflict Resolution and Ethical Oversight in Trials
Leadership in clinical research isn’t just about performance—it’s about navigating ethical gray zones and interpersonal dynamics with precision. Principal Investigators must act swiftly when conflicts arise, whether between staff, with participants, or across sponsor-site boundaries. The best PIs embed systems for both proactive conflict prevention and reactive resolution, ensuring integrity doesn’t erode under pressure.
Recognize the Root Causes of Conflict Early
Most research team conflicts don’t start explosively—they accumulate from friction points. PIs should actively monitor for:
Ambiguity in delegation or overlapping responsibilities
Misalignment between site SOPs and sponsor expectations
Personality-driven miscommunications across functions
Early identification allows subtle course correction before escalation damages morale or data flow.
Establish an Ethical Escalation Pathway
When violations, AE underreporting, or protocol concerns emerge, the escalation process must be clear, protected, and fast:
Designate a neutral team member or compliance officer for confidential intake
Formalize timelines and reporting lines for escalation to IRB, DSMB, or sponsor
Empower staff to raise flags without fear of retaliation
A clear chain of ethical escalation prevents cover-ups and delays that can lead to trial shutdowns.
Use Conflict Resolution Frameworks
Great leaders rely on frameworks—not improvisation—when tensions flare. Techniques include:
CLEAR conversations: Clarify, Listen, Explore, Align, Respond
Mediation triads: Use an uninvolved third party (e.g., regulatory manager) to de-escalate team disputes
Evidence framing: Anchor conflict discussions in objective protocol criteria or documented SOPs, not emotion
Structured dialogue preserves professionalism and minimizes bias.
Reinforce Ethical Culture through Behavior Modeling
PIs set the ethical tone more through daily conduct than declarations. That includes:
Upholding blinding procedures without exception
Immediately reporting even borderline SAEs to IRBs
Treating subjects as autonomous stakeholders—not enrollment stats
When the PI role-models integrity, ethical vigilance becomes embedded across the team.
Document and Debrief Every Ethical Event
Whether it’s a team dispute or a subject complaint, PIs must ensure:
Neutral, timestamped documentation of the event and steps taken
IRB notification logs (when required) stored for audit traceability
Internal debriefs that convert the event into a learning protocol amendment, if needed
This prevents repeat violations and demonstrates audit-ready governance.
Communication Frameworks for Cross-Functional Teams
Cross-functional clinical research teams fail not from lack of expertise—but from information gaps and misaligned assumptions. PIs who excel as communicators build layered systems of structured dialogue that flow across roles, sponsors, and trial phases. These frameworks eliminate silos and enable synchronized execution under regulatory and operational stress.
Tiered Communication Systems by Function and Frequency
Not every message should reach every team member the same way. Effective PIs establish:
Daily operational huddles for CRCs, coordinators, and on-site monitors
Weekly sponsor alignment calls led by the PI with summaries distributed to key team leads
Monthly IRB-ready reports or DSMB-prep updates, bundled with risk commentary and enrollment metrics
This cadence-based model ensures the right information reaches the right people—at the right time.
Use Asynchronous Tools to Preserve Focus
Meetings aren't always the answer. Smart PIs leverage asynchronous platforms like:
Regulatory-approved messaging tools (e.g., MS Teams with audit logs)
Shared trackers for visit logs, query resolution, and recruitment KPIs
Video memos for trial amendments, so sub-investigators can review independently
This reduces context-switching while keeping all stakeholders aligned.
Implement Communication SOPs and Handoff Protocols
Poor handoffs are a top source of protocol deviation. PIs must ensure:
Formal documentation of intra-team handoffs (e.g., from CRC to data manager)
Clear escalation steps when a handoff fails or data discrepancy emerges
SOPs for post-meeting summaries, action-item tracking, and message archiving
When communication is formalized, nothing gets lost in translation.
Promote Bidirectional Communication and Challenge Culture
Information should not only flow downward. PIs should:
Invite anonymous feedback on team communication structures every quarter
Normalize dissent by encouraging clarifying questions during sponsor meetings
Actively solicit counterarguments during protocol discussions to test for weak points
This creates a culture where team members feel safe to speak—and are trained to think critically.
Bridge External Communication Between Site and Sponsor
Many site-level errors stem from misinterpretation of sponsor intentions. Leading PIs:
Translate high-level sponsor objectives into site-specific plans
Clarify timelines, risk tolerance, and reporting expectations with mutual transparency
Act as a language bridge—turning clinical science into operational execution
Bridging this gap reduces misalignment and fosters long-term sponsor trust.
| Communication Tier | Tools & Cadence |
|---|---|
| Daily Huddles | Used for CRCs, coordinators to track on-site operations |
| Weekly Sponsor Calls | Align expectations and document trial progress updates |
| Monthly IRB Reports | Include risk analysis, AE trends, and protocol adherence reviews |
| Asynchronous Updates | Shared trackers, audit-log chat tools, and video briefings |
| Escalation SOPs | Predefined handoff protocols to prevent info loss and delays |
Metrics to Evaluate Team Efficiency and Trial Success
You can’t improve what you don’t measure. Clinical research leaders must rely on specific, actionable metrics to track both team efficiency and trial success. Without real-time indicators, hidden bottlenecks can delay timelines, jeopardize data quality, or trigger compliance violations. PIs should move beyond surface-level KPIs and instead implement a layered performance evaluation model that maps directly to outcomes.
Core Operational Metrics for Team Efficiency
The following metrics help identify internal performance issues across functions:
Protocol Deviation Rate: High deviation volume often signals poor training or communication gaps
Query Resolution Time: Tracks how fast data discrepancies are corrected, indicating cross-functional responsiveness
Enrollment vs. Forecast: Real-time tracking of recruitment against plan reveals CRC effectiveness and patient flow strategy
Visit Completion Rate on Schedule: A proxy for scheduling efficiency and site workflow coordination
PIs should review these at least weekly in fast-moving trials and monthly for long-term studies.
Compliance & Documentation Metrics
Sloppy documentation is a regulatory landmine. PIs must monitor:
Informed Consent Errors per Enrollment: A high count may point to rushed or poorly understood subject briefings
Monitoring Visit Action Items Completed On Time: Indicates site readiness and responsiveness to sponsor feedback
Audit Finding Closure Time: Tracks the duration from finding identification to documentation of corrective action
These metrics ensure audit readiness stays embedded, not reactive.
Quality-Driven Trial Success Indicators
Beyond efficiency, trial success is tied to data integrity and subject outcomes. Key metrics include:
Rate of Adverse Event (AE) Reporting Within 24 Hours: A real-time marker of ethical compliance and PI vigilance
Patient Retention Rate: Gauges trial experience quality and CRC follow-up
Data Lock Timeline Accuracy: Reflects whether upstream processes (like monitoring and cleaning) are hitting expected milestones
Tracking these ensures the trial isn’t just compliant—it’s credible.
Using Dashboards and Scorecards for Ongoing Review
PIs should consolidate all metrics into a single performance view:
Use real-time dashboards segmented by function (e.g., CRCs vs. data team)
Develop scorecards per staff member or sub-team, updated biweekly or monthly
Present trends during site meetings to celebrate wins and flag risk areas
This builds a feedback-driven culture while reinforcing accountability across every function.
| Metric Type | Example & Explanation |
|---|---|
| Operational | Protocol deviation rate flags whether your team is following the protocol consistently. Visit completion timing shows if participants are being seen as scheduled, affecting timeline reliability. Enrollment vs. forecast measures recruitment pace vs. targets, identifying CRC performance and outreach gaps. |
| Compliance | Informed consent accuracy tracks if consents are completed, signed, and dated properly—critical in audits. Audit item closure time reflects your site’s responsiveness to regulatory findings or sponsor queries. Monitoring action item completion helps ensure follow-ups after monitoring visits are executed within timeline. |
| Quality & Ethics | Adverse Event (AE) reporting speed must remain under 24–48 hours; delays indicate training or workflow issues. Patient retention rate reveals subject satisfaction and follow-through, often linked to CRC consistency. Data lock timeline accuracy shows if the trial is progressing smoothly through its final database phase. |
| Dashboarding | Create real-time dashboards segmented by function (e.g., regulatory, data, enrollment). **Scorecards per team or individual** (e.g., CRCs or data managers) offer visibility and comparison across sites or phases. Dashboards empower weekly data-driven meetings and foster shared accountability. |
| Insight Delivery | Track where delays originate, recognize overperformers, and flag early risks (e.g., sponsor dissatisfaction, patient dropouts). Feed this insight into **training sessions, SOP updates, and resourcing adjustments** to create a feedback loop. Insight metrics turn data into strategic decisions—not just compliance snapshots. |
Certification Pathway: Become a Certified Clinical Research PI (CCRPS)
Leadership in clinical trials isn’t innate—it’s built. For aspiring or current Principal Investigators aiming to master both operational excellence and regulatory command, certification is a strategic investment. The Certified Clinical Research PI program by CCRPS is one of the most targeted and comprehensive options available for developing clinical leadership capacity at scale.
Why Certification Matters for Principal Investigators
Sponsors and CROs increasingly prioritize PIs with formal training, not just years in academia or medicine. Certification:
Validates that the PI understands GCP, ICH, FDA 21 CFR, and EMA frameworks
Demonstrates operational fluency in budget management, data integrity, and protocol deviation mitigation
Serves as a career differentiator, particularly for competitive trials or global sites
In an environment where trial complexity has increased 68% over the last decade, formal training isn't optional—it’s expected.
What the CCRPS PI Certification Covers
The CCRPS Principal Investigator certification is designed around the real-world needs of PIs. It includes:
Protocol implementation, SOP creation, and advanced monitoring plan execution
Conflict resolution, IRB communications, and subject safeguarding
Site budgeting, sponsor negotiation, and compliance-centered leadership
Each module is built to meet FDA, EMA, and ICH-GCP requirements, ensuring international credibility.
Who Should Enroll?
This certification is ideal for:
Physicians entering clinical trials for the first time
Experienced PIs seeking GCP-recognized credentials
Clinical research professionals transitioning into investigator roles
Academic researchers who want to lead industry-sponsored trials
It empowers professionals to move from passive oversight to active, strategic leadership.
Frequently Asked Questions
-
Effective PIs exhibit strategic vision, regulatory fluency, and team leadership. But above all, decisiveness under pressure is what distinguishes strong trial leadership. When facing unexpected AEs, slow enrollment, or IRB concerns, a PI must act fast, using protocol-first reasoning rather than consensus delay. Emotional intelligence is also essential—a PI must resolve team friction while protecting trial integrity. These traits aren't soft skills; they're direct predictors of trial efficiency and GCP compliance. Leadership isn’t just about hierarchy—it’s about owning decisions when consequences matter.
-
A PI should implement tiered communication systems, with specific cadences for different functions. For example, CRCs may need daily huddles, while sponsors get weekly updates. Using SOP-governed handoff protocols, shared dashboards, and audit-tracked messaging tools (like Teams or Slack with logs) improves alignment. More importantly, leaders must normalize upward communication, inviting feedback and clarifying confusion early. When team members feel safe asking questions or flagging inconsistencies, protocol deviations drop and morale rises. Consistency, clarity, and feedback loops are non-negotiable.
-
Delegation means assigning tasks with oversight; abdication is dropping responsibility altogether. A PI may delegate consent briefings to CRCs, but remains accountable for ensuring every consent was properly obtained, dated, and signed. Delegation includes supervision, documentation review, and SOP adherence checks. Abdication, on the other hand, leads to missing AE reports, unsupervised site visits, or IRB miscommunication. Regulators don’t accept “I didn’t know” as an excuse—PIs must own every outcome, even when duties are shared. Smart delegation always includes traceability.
-
Even experienced PIs need formal certification because regulatory landscapes shift constantly. Sponsors now expect documented proof that a PI can lead high-stakes trials without putting data or subject safety at risk. The CCRPS Certified Clinical Research PI Program offers deep instruction on protocol execution, monitoring, and team governance—not just theoretical GCP. Certification also helps PIs expand globally, as many EMA, MHRA, or DCGI trials prefer or require training credentials. It’s not about starting from scratch—it’s about proving your leadership is compliant, current, and cross-border ready.
-
Top PIs go beyond gut feeling. They track quantitative metrics like protocol deviation rate, enrollment pace vs. forecast, and AE reporting timeframes. On the qualitative side, they measure handoff quality, role clarity, and communication consistency. Tools like dashboards, performance scorecards, and weekly feedback loops help catch early dysfunction. The goal isn’t to micromanage—it’s to build adaptive, self-correcting teams. When monitored well, even complex teams maintain alignment, reduce errors, and scale across global multicenter trials without compromising efficiency.
-
Common dilemmas include underreporting adverse events, pressure to enroll ineligible subjects, and consent inconsistencies. The correct approach is always: default to patient safety and transparency. PIs must report violations immediately to IRBs and document every decision. They should resist sponsor pressure that compromises ethics—even if it risks contract tension. Ethical leadership also means preparing your team: train CRCs to speak up, build escalation pathways, and model ethical decision-making. In trials, silence is not neutral—it’s a risk. Vigilance protects both the patient and the PI.
-
First, identify the root cause quickly—often it’s unclear roles, uneven workload, or misaligned priorities. Use structured resolution models like CLEAR (Clarify, Listen, Explore, Align, Respond) in private meetings, with a neutral party present if needed. Always document the resolution and, if relevant, adjust SOPs or workflows to prevent recurrence. PIs should maintain psychological safety—conflicts should be seen as operational issues, not personal failures. When handled swiftly and transparently, conflict can improve team cohesion and highlight process gaps, instead of harming data integrity.
-
They confuse authority with leadership. New PIs often assume their title guarantees team alignment, but in reality, clinical teams follow clarity, not rank. Without proper onboarding, defined workflows, and feedback channels, teams falter—even if led by MDs or PhDs. The biggest mistake is assuming everyone "knows what to do." The solution? Treat leadership like protocol management: structured, documented, and constantly monitored. Build systems that run without you, but still hold your oversight. That’s the hallmark of sustainable, audit-proof trial leadership.
Final Thoughts
Leadership in clinical research doesn’t come from academic titles—it’s earned through proactive strategy, ethical clarity, and people-centered systems. Principal Investigators who manage high-performance teams don’t just deliver clean data—they create sustainable trial ecosystems that sponsors trust, subjects feel safe in, and teams want to stay part of. The gap between an average PI and a standout leader is rarely about credentials—it’s about how consistently they build, communicate, and correct under pressure.
If you're ready to lead clinical research teams at the highest level, it’s time to formalize your skills through advanced training. Programs like the CCRPS Certified Clinical Research PI certification empower you to not only manage trials—but to lead them with precision, compliance, and impact. Because in modern clinical research, leadership isn’t optional—it’s regulatory armor.