The Ultimate Guide to Clinical Research Monitoring
Clinical research monitoring plays a crucial role in the success of clinical trials, encompassing diverse activities to guarantee the safety and precision of collected data. The execution of clinical trials must adhere to regulatory standards, prioritize the protection of human study participants, and minimize potential health risks. Monitoring activities include auditing study sites, assessing data accuracy and completeness, protocol and amendment reviews, scrutiny of case report forms (CRFs), identification of deviations from standard operating procedures (SOPs) or protocols, management of corrective action plans (CAPs), safety report follow-ups, and tracking progress against enrollment goals.
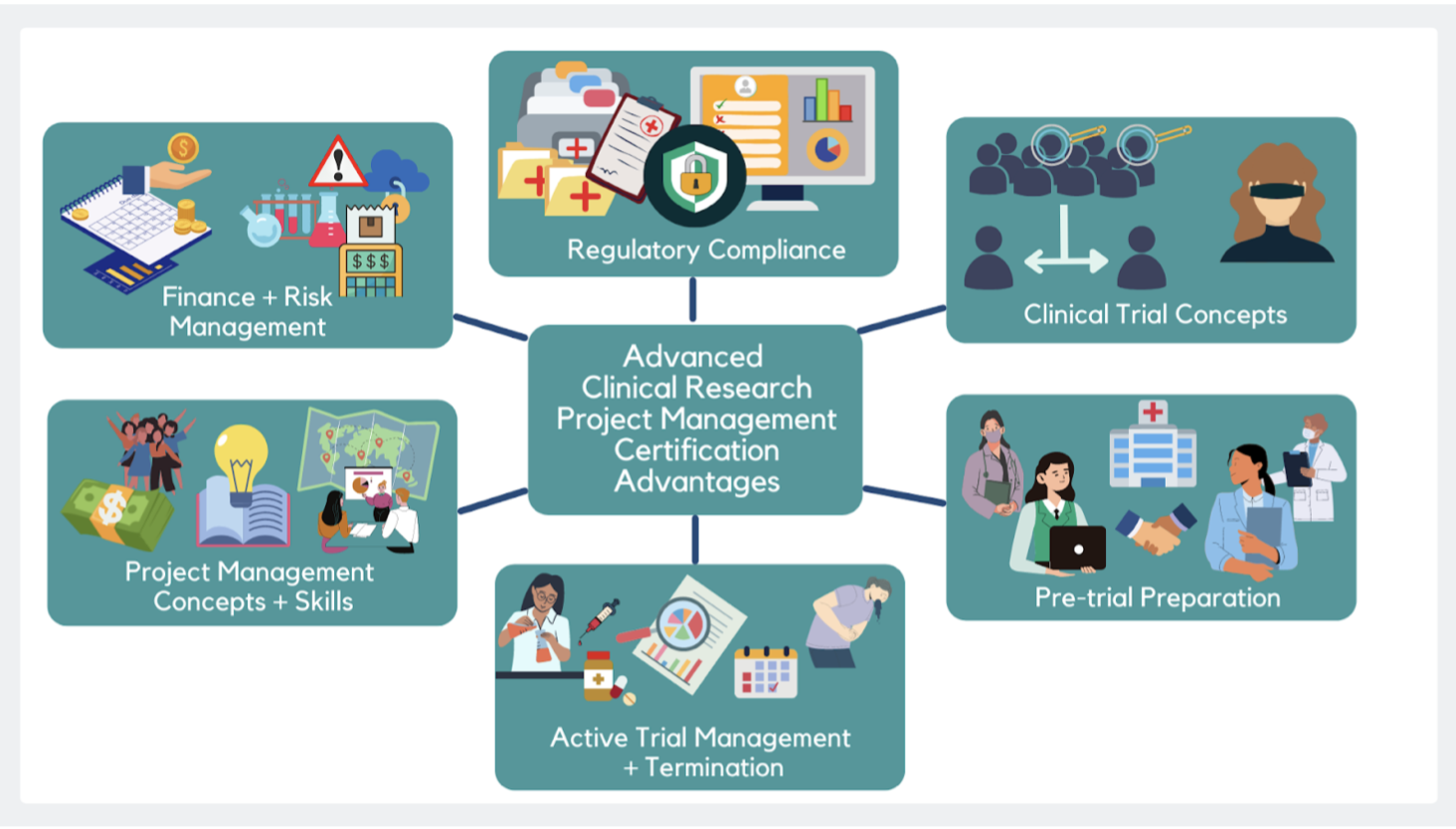
For those interested in becoming involved in clinical trial management and oversight, the Advanced Clinical Research Project Manager Certification offers extensive training in these key areas.
Beyond data quality assessment, clinical research monitoring ensures compliance with regulatory standards such as GCP (Good Clinical Practices), ICH (International Conference on Harmonization), FDA regulations, and local laws. Those looking to deepen their understanding of these standards might find the ICH-GCP course particularly beneficial. Ongoing monitoring throughout a study, coupled with potential audits by sponsors or regulatory authorities, contributes to the accuracy, reliability, and applicability of clinical trial results for informed medical decisions.
Steps to Clinical Monitoring:
Craft a Robust Monitoring Strategy: Develop a thorough monitoring plan encompassing essential elements. This includes specifying the types of monitoring activities, setting the frequency of monitoring visits, outlining data collection methods, and establishing clear criteria for acceptable performance.
Aspiring Clinical Research Coordinators can enhance their strategy formulation skills through the Clinical Research Coordinator course.
Create Effective Documentation: Develop monitoring tools tailored to the protocol, including forms for recording information from site visits, source documents, data collection instruments, and case report forms (CRF). Additionally, establish a Monitoring Log or Tracking System to enhance accountability for study activities.
For detailed training on documentation practices, consider the Clinical Trials Assistant Training.
Conducting Monitors' Visits: Depending on the trial's complexity and regulatory mandates, execute pre-study qualification visits (PSQV), pre-initiation visits (PIV), initiation visits (IVs), periodic monitoring visits (PMV), and close-out visits (COV). Throughout each visit, uphold good clinical practice standards by thoroughly reviewing source documents and data collection instruments. Scrutinize patient enrollment logs for accuracy, noting any discrepancies in the comprehensive visit report.
The CRA course provides in-depth training for those looking to conduct these critical visits.
Reporting Findings: Create comprehensive yet succinct reports after each monitor's visit, offering clear recommendations for corrective actions as needed. Provide professional feedback to investigators, highlighting their performance. Identify and address any noncompliance with protocol requirements or regulations, suggesting training or educational sessions when necessary. Track all follow-up activities related to corrective actions taken in response to monitor's visit findings. Ensure the completion of essential documentation before closing out a specific study site.
Those interested in the oversight of safety reporting might explore the Pharmacovigilance Certification.
Ensuring Quality Assurance: Validate the accuracy of tracking systems employed by monitors during their visits. Assess the risks linked to identified deficiencies throughout the monitoring process. Conduct regular internal audits/assessments to guarantee compliance with established SOPs/guidelines pertaining to clinical research monitoring activities. Implement preventive measures based on audit/assessment results to enhance internal quality system processes.
Professionals aiming for a specialized role in this field might consider the Medical Monitor Certification.
Types of Clinical Trial Monitoring
Onsite Monitoring: Onsite monitoring, considered the "gold standard," entails a monitor's presence at a study site throughout the trial. The monitor reviews source documentation, including patient records, lab results, and investigational product dispensing logs, ensuring accuracy and compliance with study protocols and good clinical practices (GCP). Staff interviews verify proper adherence to trial procedures.
Centralized or Remote Monitoring in Clinical Trials: Centralized or remote monitoring allows sponsors to conduct clinical research monitoring without onsite visits. Leveraging technology like web portals and video conferencing, monitors remotely review data from multiple sites simultaneously. This method facilitates quick issue identification. Moreover, it enables proactive risk assessment before onsite visits, enhancing the efficiency of the monitoring process.
Types of Clinical Research Monitoring: Clinical research monitoring is a critical process that evaluates the quality and integrity of clinical trial data, ensuring adherence to regulatory requirements. Three primary methods are employed: onsite monitoring, centralized or remote monitoring, and risk-based approaches.
4. Risk-Based Approaches (2024): Embracing the advancements of 2024, risk-based approaches now leverage cutting-edge data analytics tools like advanced descriptive statistics and predictive algorithms. These tools identify potential trends or outliers in clinical trial data, signaling an increased risk of noncompliance with Good Clinical Practices (GCPs) or other regulations. Technology-driven approaches enable sponsors to detect issues earlier in a trial, allowing timely corrective action to prevent complications.
5. Benefits of Clinical Research Monitoring (2024): In the ever-evolving landscape of clinical research, effective monitoring strategies play a pivotal role in ensuring trials are conducted ethically, safely, and in accordance with protocol standards. Aligned with timelines agreed upon with regulatory authorities and budget constraints set by sponsors/CROs/investigators, these strategies provide invaluable insights. Acting as independent third parties, clinical research monitors offer objective perspectives across multiple sites, minimizing biases from investigators or personnel with vested interests.
Furthermore, contemporary monitoring ensures patient safety by overseeing the administration of drugs or medical devices and maintaining confidentiality throughout the study. Robust monitoring protocols also prove instrumental in reducing costs associated with potential delays, preventing errors throughout the trial duration, from pre-study startup to post-closeout when all enrolled patients have completed their participation.
Clinical Research Monitoring Guide
1. Mastering Clinical Research Monitoring in 2024:
Dive into the core of clinical research monitoring, a vital aspect of the research process ensuring both safety and result accuracy. Regular assessments of study sites verify proper data collection in adherence to ethical standards, legal requirements, and the latest Good Clinical Practice (GCP) guidelines.
2. Demystifying Monitored Study Types:
In the SEO landscape of 2024, clinical research monitoring extends beyond clinical trials to encompass observational studies, epidemiologic studies, and public health surveys. Understanding the specific study type being monitored is crucial for ensuring the correct procedures are implemented.
3. Navigating Study Site Monitoring:
Stay current with 2024 SEO standards by comprehending the intricacies of clinical research monitoring. The primary objective is meticulous confirmation that both protocol and informed consent forms are followed at each site. This involves in-depth reviews of relevant documents such as case report forms (CRFs), source documentation (e.g., physician notes), internal audit reports, and external quality assurance reports. Compliance with GCP guidelines during site visits or remote reviews, coupled with interviews assessing data collection and reporting processes, enhances the monitoring process.
4. Grasping Regulatory Requirements in 2024:
Beyond GCP guidelines, the SEO-friendly approach for 2024 emphasizes an awareness of applicable regulations from local governments or institutions. Adherence to these regulations is vital for compliance with laws related to clinical research monitoring activities.
5. Crafting an Advanced Monitoring Plan:
Elevate your monitoring plan in 2024 with a detailed timeline for site visits, specific focuses (e.g., patient enrollment/randomization, adverse event management), and strategies for auditing/reviewing generated data. Incorporate measures to control data collection risks, enabling early issue identification, aligning with SEO standards and ensuring a smooth study process.
Clinical Research Monitor Job
A Clinical Research Monitor plays a crucial role in ensuring the ethical and safe conduct of clinical trials while maintaining compliance with established standards. The primary focus is safeguarding the rights, safety, and well-being of human subjects participating in the trials. Responsibilities encompass a wide range of activities, including protocol development, coordination of study start-up, site visits, monitoring data accuracy and completeness, auditing files for regulatory compliance, managing investigator queries, preparing visit reports, reviewing protocol updates, resolving issues identified through audits, offering technical guidance to sites on protocol implementation, and escalating complex issues or potential risks.
Clinical Research Monitor Salary
The salary for this position varies based on factors such as education, experience, and geographical location. Entry-level positions may start at around $60,000 per year, while experienced professionals can earn up to approximately $90,000 per year. In addition to salary, many employers provide benefits such as paid vacation days, health insurance plans, and retirement packages.
Resources for Clinical Research Monitoring
1. National Institutes of Health (NIH): Clinical Research Monitoring
This link provides information on NIH's guidelines for monitoring clinical research, which include topics such as the roles and responsibilities of the investigator, data safety monitoring boards, and protocols for reporting unanticipated problems and adverse events.
2. National Institutes of Health (NIH): Guide to Clinical Research Monitoring
This comprehensive guide walks readers through all aspects of clinical research monitoring, including topics such as study design, randomization strategies, regulatory compliance requirements, data management, monitoring plans and reports, quality improvement initiatives, and safety assessments.
3. US Food and Drug Administration (FDA): Guidelines for Clinical Trials Monitoring
This resource from the FDA outlines the importance of effective monitoring in clinical trials and provides an overview of the different roles within a clinical trial as well as details about essential elements for implementation of an effective monitoring strategy such as risk assessments and adverse event tracking.
4. International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH)
ICH has developed standards that provide a set of harmonized technical requirements for clinical trials conducted across countries in the European Union (EU), Japan, and US with an emphasis on quality assurance and safety monitoring during trials.
5. Association of Clinical Research Professionals (ACRP)
ACRP's guidelines provide best practice recommendations for conducting clinical research studies in accordance with applicable regulations and standards to ensure patient safety monitoring during studies as well as data integrity throughout the process from start to finish.
6. Pharmaceutical Research & Manufacturers of America (PhRMA)
The PhRMA guidelines provide an overview of expectations around clinical research activities with respect to ethics, data integrity, safety reporting, resource allocation and more. It defines roles and responsibilities of all those involved in overseeing a clinical trial such as a Clinical Research Monitor or CRA who has primary responsibility for ensuring that the protocol is implemented correctly throughout a study’s duration
Clinical Research Monitoring Review
1. What is the main purpose of clinical research monitoring?
A) To ensure that a research study is conducted in accordance with applicable regulations and ethical standards
B) To ensure that data collected during a research study is accurate and reliable
C) To evaluate the safety of participants enrolled in a research trial
D) To oversee the financial management of a research project
Answer: A) To ensure that a research study is conducted in accordance with applicable regulations and ethical standards. Clinical Research Monitors are responsible for ensuring compliance with Good Clinical Practice guidelines, protecting participant privacy, verifying data accuracy, and evaluating protocol deviations. In addition, they may also be involved in reviewing participant eligibility requirements, conducting site assessments, providing training to investigators and staff on proper study procedures, as well as monitoring progress towards completion of all requirements of the study.
2. What type of individuals typically serve as clinical research monitors?
A) Physicians
B) Nurses
C) Regulatory specialists
D) All of the above
Answer: D) All of the above. Clinical Research Monitors can come from various backgrounds such as medical doctors (MDs), nurses (RNs), pharmacists (RPhs), regulatory specialists (e.g., Regulatory Affairs Professionals or Paralegals), or biostatisticians/data analysts who have experience in clinical trials and understand local regulations related to human subject protection. Each monitor has specific job duties depending on their education and experience, such as assessing compliance with regulatory guidance or analyzing data sets for accuracy, completeness, integrity, or validity.
3. What kind of activities do clinical research monitors need to perform?
A) Protocol reviews or verifications
B) Ensuring appropriate documentation completion
C) Site visits to observe investigator conduct
D )All of the above
Answer: D )All of the above. Clinical Research Monitors need to perform several activities including protocol reviews or verifications; ensuring appropriate documentation completion; site visits to observe investigator conduct; liaising between sponsors and sites; assisting with resolving issues associated with adverse events; reviewing case report forms for completeness, accuracy, consistency and correctness; evaluating subject safety throughout enrollment process;and writing reports detailing their findings at each visit.
4. What is one benefit gained from having an effective Clinical Research Monitor on-site? A) Reduced risk for legal liability stemming from negligence
B) Improved protocol adherence by investigators
C) Increased patient engagement during trial period
D )All of the above
Answer: D) All of the above . An effective Clinical Research Monitor encompasses several benefits such as reduced risk for legal liability stemming from negligence due to thorough oversight and accurate record keeping; improved protocol adherence by investigators through continued communication between sponsor representatives and researchers on-site regarding best practices; increased patient engagement during trial period due to more detailed explanations about potential risks/benefits offered by having monitor on-site ; and improved efficiency when dealing with complex protocols that require multiple levelsof oversight due to familiarity with protocol specifics which decreases time spent troubleshooting errors or unclear instructions..
5. How often should Clinical Research Monitors visit a particular site?
A) Weekly B) Biweekly C) Monthly D) Quarterly
Answer: C) Monthly . It is recommended that Clinical Research Monitors visit sites at least once per month in order to maintain active surveillance over ongoing studies at each location while also providing timely feedback regarding any issues discovered while on-site visits are taking place within a shorter timeframe if needed based upon changes made midstream or other unanticipated circumstances which might require immediate attention by sponsor personnel.
Clinical Research Project Manager
Clinical Research Project Manager - A Full Guide To Becoming a Clinical Trial Project Manager
As of mid-April 2022, top recruitment platform ‘indeed.com’ lists 6,026 openings for Clinical Research Project Managers across the United States[1]. According to ‘payscale.com’, remuneration for this profile ranges from $84,168 for early-career to $120,501 for experienced Clinical Research Project Managers, with a mid-career median of $107,649[2].
A Clinical Research Project Manager (henceforth CRPM) is also known as a Clinical Research Manager or a Clinical Trial Manager. The role of a CRPM is to provide leadership during the clinical trial of new drugs, with the overarching goal of ensuring that the clinical trials process is completed within the stipulated time-frame and allocated budget, while maintaining the highest standards of research quality and scientific integrity.
An overview of the CRPM profile
A Clinical Research Project Manager is the liaison between the study sponsor and the clinical research team. Thus, the CRPM must balance the expectations of the funding organization in a clinical research study (pharmaceutical company, governmental agency, university research division or other entity) with the needs of the team, including Principal Investigators (PIs) and co-PIs, Clinical Research Coordinators (CRCs), Clinical Research Associates (CRAs), and Clinical Trial Assistants (CTAs) and other site staff.
The CRPM plays a leading role in planning, implementation and ongoing monitoring of live clinical trials. In the process, a CRPM also mentors junior team members, including CRAs and CTAs.
Evidently, a career as a CRPM is rewarding, but also demanding. So, what does it take to qualify and be recruited as a Clinical Research Project Manager?
The road-map to becoming a CRPM
Even if you’re new to the field of clinical research, you’ve probably guessed by now that becoming a Clinical Research Project Manager takes both qualifications and experience. A typical CRPM has a bachelor’s (or master’s) degree in life science, combined with four to five years’ experience in one or more clinical research roles such as CRC, senior CRA or QPPV (Qualified Professional in Pharmacovigilance).
Irrespective of where you are along this path, the remainder of this article charts a clinical research professional’s journey of growth in developing into a competent CRPM. For conceptual convenience, the process is discussed in two parts – Part 1 centers on the research and administrative skills needed for a CRPM, while Part 2 revolves around expertise in project management. The final sections address how the Advanced Clinical Research Project Manager Certification or ACRPMC facilitates the transition to a CRPM role.
The CRPM journey, Part 1: Research and administrative skills
By the time a clinical research professional is eligible to apply for a CRPM position, s/he has typically developed a range of competencies in the day-to-day running of clinical trials. In addition, a professional at this stage has usually acquired a good working knowledge of the planning and oversight required for a clinical research study.
In broad strokes, a CRPM candidate likely already has a knowledge base and skill sets in the following areas:
1. ICH-GCP guidelines, Title 21 of FDA CFR and IRB compliance
One of the first things every clinical research professional learns is the importance of adhering to the principles and policies of good clinical practice, as outlined in the ICH-GCP[3]—these guidelines set the framework for carrying out research in a manner that prioritizes the safety and welfare of human subjects and the quality and integrity of clinical data.
The ICH-GCP principles are mirrored by Title 21 within the US FDA’s Code of Federal Regulations (CFR)[4]. Clinical research across the US must conform to the requirements of Title 21. Part of Title 21 regulatory compliance requires nearly all clinical research studies to first be approved by an Institutional Review Board or IRB (also called an Ethics Committee). As clinical trials progress, any changes to the study trial protocol, consent procedures or data management system must likewise first be reviewed and approved by the IRB.
The CRPM has final responsibility for ensuring that all documentation necessary for clinical research regulatory compliance is maintained and updated as needed.
2. Clinical trial design concepts and parameters
A sound grasp of the clinical trials process is similarly a must for senior professionals in the team. Candidates for CRPM positions are thus expected to have a thorough understanding of key concepts and procedures relating to clinical research, including:
Phases 1 to 4 of clinical trials[5]
Investigational products (IPs) including INDs and IDEs
Design concepts in clinical trials - control, randomization and blinding
Subject screening and selection, retention and study compliance
Trial data input, quality assurance, analyses and reporting
Adverse Event (AE) documentation and reporting
3. Pre-trial preparation
In some ways, the most crucial phase of a clinical trial is the preliminary or preparatory phase, during which all groundwork must be laid for the smooth and efficient conduct of the actual study. This phase must typically achieve the following objectives:
Complete documentation for initiating clinical trials[6] – An IRB-approved clinical trial must have in place a host of documents covering important aspects of the study, including the investigator brochure (IB), trial master file (TMF), informed consent form, case report form (CRF), subject recruitment notice, laboratory protocol, study financial projections and so on.
Identification and preparation of study site(s) – Most clinical research studies are run across multiple sites, which may be hospitals, clinics or other health-care facilities. Identifying suitable sites, establishing collaborative agreements with site administrators, as well as setting up the required infrastructure to carry out trials at each site is crucial in preparing for a clinical research study.
Pre-trial publicity – The success of clinical trials depends on gathering large amounts of data from human subjects. Therefore, creating public awareness and interest right from the outset is critical to running clinical research studies effectively.
When setting up a study, the CRPM plays a central role in initiating and fulfilling each of the goals outlined above. Under the CRPM’s guidance, clinical research administrative staff including CRCs and CRAs work to put relevant documentation in place, prepare study sites and create public awareness about the study.
4. Active trial administration
The day-to-day running of an active clinical trial involves numerous administrative components, including:
hiring and training staff at clinical sites
tracking subject recruitment and retention
regulatory compliance in trial protocol, subject safety and data quality
Adverse Event (AE) documentation and reporting
oversight of trial drug storage and use
coordination among research teams across sites
tracking study finances
communication between study sponsors and clinical staff
electronic data capture (EDC) and management
timely renewal of necessary financial and regulatory approvals
These tasks are distributed among members of the investigative teams (PIs, co-PIs and other medical personnel) as well as administrative teams (CRAs, CRCs, QPPVs and other site staff). However, the CRPM is ultimately responsible for ensuring efficient administration that keeps the clinical trial on track.
5. Study termination procedures
Winding up a clinical trial similarly entails a number of administrative exercises. Here again, the CRPM must oversee execution, guiding team members in completing tasks on schedule and to the required standard:
site close-out (relieving staff, subject debriefing, equipment surrender)
final data consolidation and scrutiny
study completion documents for regulatory compliance
compilation of briefs and reports for regulatory authorities, study sponsors
The CRPM journey, Part 2: Expertise in project management[7]
Most aspirants to CRPM positions have usually been engaged in the clinical research process for at least a few years. Many have played administrative roles, working as CRCs, senior CRAs, QPPVs or site managers. In some cases, CRPM aspirants have clinical backgrounds, with expertise in drug research or medical monitoring.
Despite their hands-on experience with the clinical trials process, professionals wishing to transition to CRPM roles usually have limited exposure to the higher-level project management knowhow that is essential for an effective CRPM. This section provides a brief overview of the major project management domains relevant to clinical trial management:
1. Project and operations planning
A clinical trial is a major operation, involving a range of geographical and health-care settings, multi-disciplinary teams, as well as a complex array of regulatory and logistical requirements. Planning the stages, milestones and operations of a clinical trial is integral to assuring its success. Therefore, project and operations planning are the top priorities of a CRPM.
Some of the key elements involved in planning a clinical trial include:
Compiling a comprehensive study protocol describing the rationale, aims, design and methodology, data analysis plans, and trial procedure (/protocol)
Setting project goals, deliverables and milestones
Outlining a project personnel schematic that delineates team and sub-team structure and defines individual team member roles
Generating a responsibility blueprint with a clear break-up of tasks, targets and time-lines for each project goal and each team member
Creating a communication plan that outlines the method and schedule for relaying information, updates and requests between and within teams
2. Financial forecasting and tracking
One of the biggest challenges confronting a CRPM is keeping the trial within budget, while making sure that resources are optimally allocated to cover all necessary project-related expenses. Clinical trials often suffer from scope creep, that is, the inclusion of additional goals and deliverables to those originally outlined, resulting in the project overshooting budget and time-line.
It is therefore recommended practice for a CRPM to work with study sponsors and senior team members in compiling a budget management plan at the very outset of the project. Such a plan not only specifies financial outlay for each of the goals and deliverables of the clinical trial, it also provides for periodic budget revisions to account for factors such as expanded project scope, rising costs and supply-chain changes.
3. Human resource allocation and oversight
The section on project and operations planning highlighted the importance of creating a personnel schematic as well as a responsibility blueprint at the start of a clinical trial. Through this process, a CRPM is able to clearly define roles for various team members in meeting project goals and milestones, and their contributions to each project deliverable.
However, in order to ensure collaborative effort and a cordial work environment, it is essential for a CRPM to also formulate a transparent hiring policy as well as disciplinary policy. These may be specific to the clinical trial or apply broadly across the CRO, or Clinical (/Contract) Research Organization. Well-documented policies facilitate the CRPM’s role in sourcing and motivating the best-fitted staff to play different roles in the clinical team.
4. Clinical data management and quality control
The data from a clinical trial are often its most valuable project outcome. As such, effectively managing the input, storage, analysis and quality control of study data is one of the foremost responsibilities of a CRPM.
Before beginning the active phase of the clinical trial, a CRPM coordinates with team members to put in place the following aspects of data management:
physical data storage system (files, binders, shelves, cabinets, etc.)
electronic data capture (EDC) and management system
physical and electronic data security systems
data input procedure
data cleaning and quality monitoring procedure
data sharing (import, export, access across clinical sites and teams)
data analysis and visualization procedure
periodic data review and reporting procedure
5. Risk management and mitigation
Owing to the high stakes nature of clinical research, running a clinical research study carries numerous risks. One of the major responsibilities of a CRPM is to develop a risk management plan to identify and circumvent potentially risky situations, and to mitigate consequences to the project in cases where an unforeseen risk impacts the trials process.
Some sources of risk in the management of a clinical trial include:
failure to obtain or document subject informed consent
errors in following trial protocol (timing, dosage, subject screening, etc.)
data security breach leading to compromised subject confidentiality
inadequate insurance coverage for potential adverse events of study
financial constraints arising from changes in study funding
limitations on study scope due to revisions in regulatory policy
Bridging the gap: Using ACRPMC to transition from clinical research professional to project manager
The foregoing section outlined how, despite their strong base in clinical research, CRPM aspirants generally lack the advanced knowhow and managerial skills required for leading a clinical research project. CCRPS’ Advanced Clinical Research Project Management Certification (ACRPMC) provides an excellent tool for bridging this gap and bringing candidates up to speed in all domains of clinical research management.
The table below offers a summary of the focus areas of the ACRPMC, detailing how each contributes to enhancing a candidate’s expertise and eligibility for the role of a Clinical Research Project Manager.
ACRPMC Focus Area |
Contribution to CRPM Candidate Eligibility |
ADVANCED REVIEW - I: Regulatory compliance in clinical research |
i.Fundamentals of subject (/patient) safety, ICH-GCP E6, Sections 2 - 4 |
ii.Regulatory compliance – FDA-CFR Title 21, Forms FDA 1571, 1572, 3454, 3455 |
|
iii.Investigational New Drug (IND) & New Drug Application (NDA), Investigational Device Exemption (IDE) |
|
iv.IRB, Data Safety Monitoring Board (DSMB)[8] |
|
ADVANCED REVIEW - II: Clinical trial concepts |
i.Process & phases of clinical testing (pre-clinical and phases 1 to 4) |
ii.Importance of ‘control’ in testing[9], outcome validity, control methods (randomization, blinding) |
|
iii.Subject (/patient) selection[10]: screening & exemption criteria, selection & retention, study compliance |
|
iv.Clinical trial data management[11]: EDC, Clinical Trial Management Systems (CTMS), Interactive Response Technology (IRT), Randomization & Trial Supply Management (RTSM) |
|
v.Subject safety[12]: Risk assessment & Individual Case Safety Reports (ICSRs), Adverse Events (AEs), Adverse Drug Reactions (ADRs), Important Medical Events (IMEs) |
|
ADVANCED REVIEW - III: Pre-trial preparation |
i.Documentation[13]: Regulatory binder, Investigator Brochure (IB), Trial Master File (TMF), Case Report Form (CRF), Delegation of Authority Log (DOAL), etc. |
ii.Site preparation[14]: Site Selection Visits (SSVs), Site Qualification Visits (SQVs), site management agreements, investigator selection |
|
iii.Pre-trial publicity: Advertisement for subject recruitment & retention |
|
ADVANCED REVIEW - IV: Active trial management & trial termination |
i.Clinical trial protocol compliance, deviations & violations |
i.Clinical site monitoring: subject safety, drug storage & safety, regulatory compliance |
|
ii.Data monitoring: data security & access, Quality Management System (QMS), Quality Control (QC), Key Quality Indicators (KQI) |
|
iii.Team monitoring: communication & collaboration, adherence to trial & safety protocols, research integrity & fraud |
|
iv.Reviews & audits[15]: document & site audits, data audits, financial audits |
|
v.Study termination: site close-out visits, data consolidation, subject debriefing |
|
EXPERTISE BUILDING - I: Clinical project management fundamentals |
i.Project management basics[16]: key concepts, Project Management Body of Knowledge (PMBOK) |
ii.Skills of a project manager: technical, administrative, human resources, public relations |
|
iii.Clinical project stakeholders: sponsors, IRB, investigative & administrative staff, site administrators |
|
EXPERTISE BUILDING - II: Advanced clinical project management |
i.Project planning & tracking, progress evaluation metrics |
ii.Financial management[17]: project budgeting, site budgeting, advertising budget, payment tracking and management |
|
iii.Risk management & problem solving[18]: problem solving managerial skills, identifying risks, avoiding failures, resolution of project problems (protocol deviations, compliance failures, project delays) |
Fast-track to CRPM with the ACRPMC advantage
From the above summary table, it can be seen that the ACRPMC[19] program of CCRPS covers the entire spectrum of competencies required for managerial clinical research professionals. In addition to providing in-depth training in clinical project management concepts, tools and techniques, the program includes a review of foundational as well as advanced knowledge of the clinical trials process.
Aside from its comprehensive curriculum, certification through ACRPMC offers major benefits over conventional clinical research management courses, both online programs as well as those offered by colleges and universities. Some of the outstanding advantages of ACRPMC are:
1. Foundational review plus advanced training
The ACRPMC program stands apart from other online programs in its unique ability to launch as well as advance careers in clinical research. The program is equally effective at helping an aspiring graduate (BA in science or BS degree) to gain a competitive advantage in the clinical research job market, as it is at catapulting a senior clinical researcher into a managerial position.
For CRPM aspirants in particular, the ACRPMC provides an unrivaled opportunity to brush up on the basics, in addition to acquiring valuable knowhow in clinical research project management, before embarking on the applications and interview process.
2. Over 100 training modules (250 hours of coursework)
The course comprises over 100 modules. The advanced review focus areas address all aspects of the clinical research process, including important investigative concepts (trial design, randomization, subject screening, data analysis, etc.) as well as administrative processes (maintenance and updating of regulatory documents, case reports, trial logs, etc.). Additionally, the expertise building focus areas of the ACRPMC cover basic and advanced project management concepts and skills that equip candidates to tackle the challenges of leading a clinical research study.
3. ICH-GCP E6R2 compliant
Designed by experienced Clinical Research Project Managers, the ACRPMC curriculum is fully compliant with the regulatory requirements of the ICH-GCP E6R2. The course coordinators additionally ensure that the content is regularly updated to reflect revisions to policy and new requirements.
4. Immediate enrollment and fast-tracked certification
Unlike college and university courses, trainees can enroll in the ACRPMC with just a few clicks. In addition, the self-paced course design allows students to skim through familiar topics, while giving more time and attention to new material. This is especially advantageous for working professionals and senior clinical research professionals wishing to refresh their knowledge. Trainees able to dedicate several hours per day to the program can complete the ACRPMC in as little as two weeks.
5. Multiple accreditations and industry-wide recognition
For ACRPMC-certified trainees, the solid credentials of the program confer a huge benefit when applying and interviewing for clinical research positions. Like other CCRPS courses, the ACRPMC is also accredited to ACCRE (Accreditation Council For Clinical Research and Education), ACCME (Accreditation Council for Continuing Medical Education) as well as ACPE (Accreditation Council for Pharmacy Education).
6. Clinical research résumé building and interview preparation
The final modules of the ACRPMC help trainees in building their ability and confidence to face interviews for clinical research positions. Trainees completing the comprehensive final examination not only have immediate access to a digital certificate, but are eligible to receive a letter of recommendation (LoR) that can strengthen their clinical research job application.
As the clinical research industry continues to grow at an unprecedented pace, there is rising demand for Clinical Research Project Managers who can blend their skill and experience in clinical research with savvy, expert project management abilities. As a professional clinical researcher, the ACRPMC program offers you an unmatched opportunity to refresh existing knowhow and acquire new competencies, thereby leveraging your rise to the top echelons of management.
If you are a fresh graduate, the ACRPMC represents an unequaled, early-career edge in the clinical research arena. By equipping you with foundational as well as advanced knowledge and skills, ACRPMC certification does not merely improve your chances of securing an attractive clinical research position, it assures the rapid upward growth of your career graph.
Advanced Clinical Research Project Manager Certification (ACRPMC) program advantages.
References
https://www.indeed.com/jobs?q=Clinical%20Trial%20Manager&l&vjk=311beece3c2d98b6
https://www.payscale.com/research/US/Job=Clinical_Trial_Manager/Salary
Dixon JR. 1999. The international conference on harmonization good clinical practice guideline. Quality Assurance. 6(2): 65-74. DOI: 10.1080/105294199277860
https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm?fr=312.32
https://ichgcp.net/8-essential-documents-for-the-conduct-of-a-clinical-trial
Cullen H. 2016. Effective project management for clinical trials: A business approach. Ebook: https://www.imperialcrs.com/files/Project_Management_Ebook_Final.pdf
Jüni P, Altman DG, Egger M. 2001. Assessing the quality of controlled clinical trials. BMJ. 323(42). DOI:10.1136/bmj.323.7303.42
Farrell B, Kenyon, S, Shakur H. 2010. Managing clinical trials. Trials 11(78) DOI:10.1186/1745-6215-11-78
von Itzstein MS, Hullings M, Mayo H, Beg MS, Williams EL, Gerber DE. 2021. Application of Information Technology to Clinical Trial Evaluation and Enrollment: A Review. JAMA Oncol. 7(10):1559–1566. DOI:10.1001/jamaoncol.2021.1165
Yao B, Zhu L, Jiang Q, Xia HA. 2013. Safety Monitoring in Clinical Trials. Pharmaceutics. 5(1):94-106. DOI: 10.3390/pharmaceutics5010094
https://files.nccih.nih.gov/s3fs-public/CR-Toolbox/Regulatory_Binder_Checklist_ver3_07-17-2015.docx
https://www.appliedclinicaltrialsonline.com/view/selecting-study-appropriate-clinical-sites-3-steps
https://www.clinicaltrialsarena.com/news/how-to-prepare-for-an-fda-site-inspection-5739632-2/
PMBOK® Guide (7th ed.). 2022. Project Management Institute.
Appleson M. 2015. The importance of budgeting in clinical trials and how a budget can prevent billing errors. Clin Invest. 5(5): 437-439. DOI: 0.4155/CLI.15.11
Robinson M. 2005. Clinical trials risk management (1st ed.). CRC Press. DOI: 10.1201/9781420037654
https://app.ccrps.org/courses/Advanced-Clinical-Research-Project-Manager-Certification