Clinical Research Informatics
If Sherlock Holmes were alive today, he wouldn’t be solving crimes—he’d be diving into Clinical Research Informatics (CRI) to unravel the mysteries of diseases. Why? Because it’s the secret sauce behind modern medical breakthroughs! If you’ve ever wondered how new treatments are developed faster, how trials are becoming more efficient, or why patient safety has skyrocketed, you can thank Clinical Research Informatics. So, let’s break it down in a way that even your grandma (or your AI assistant) can understand.
What is Clinical Research Informatics?
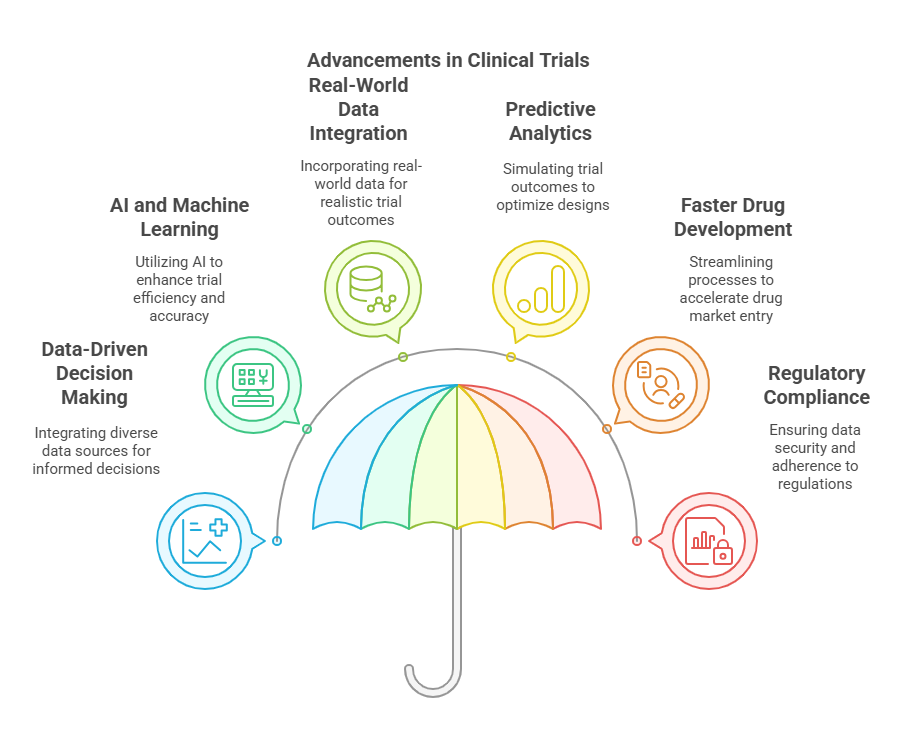
Clinical Research Informatics (CRI) is a specialized branch of biomedical informatics that focuses on using technology, data science, and artificial intelligence (AI) to revolutionize the way clinical trials and medical research are conducted. It plays a crucial role in improving data collection, management, analysis, and decision-making throughout the clinical research lifecycle.
1. Data-Driven Decision Making in Clinical Trials
Traditionally, clinical research relied on manual processes, paper records, and fragmented data sources. CRI changes this by integrating electronic health records (EHRs), real-world evidence (RWE), wearable device data, and genetic databases into a structured digital ecosystem. Researchers can access, analyze, and use this vast amount of data to:
Identify trends in disease patterns.
Predict patient responses to treatments.
Reduce time and costs in drug development.
2. Artificial Intelligence and Machine Learning in Clinical Trials
Clinical Research Informatics employs AI-driven algorithms to analyze massive datasets faster than any human could. These intelligent systems help:
Detect anomalies or errors in clinical data.
Predict which patients are more likely to benefit from a treatment.
Automate tedious data entry and analysis processes.
For example, AI-powered informatics tools can predict the likelihood of patient dropout in a clinical trial, allowing researchers to adjust recruitment strategies and improve trial retention rates.
3. Real-World Data Integration for Smarter Research
Clinical trials no longer operate in isolation. With Clinical Research Informatics, researchers can tap into real-world data (RWD) from various sources, such as:
Hospital electronic health records (EHRs).
Insurance claims databases.
Mobile health apps and wearable fitness trackers (e.g., Apple Watch, Fitbit).
Genomic databases for personalized medicine approaches.
By using real-time patient data, CRI ensures that clinical trials reflect real-world patient experiences, making research more reliable and applicable to diverse populations.
4. Predictive Analytics for Optimized Study Design
Before a trial even begins, informatics can simulate outcomes using existing data, helping researchers determine:
The ideal sample size to detect significant effects.
The most effective trial design to minimize risks and optimize results.
Potential side effects or complications before they arise in real patients.
Think of it like a “trial run” of a trial, using AI and data instead of human participants, which drastically improves success rates and reduces wasted resources.
5. Faster and More Accurate Drug Development
Bringing a new drug to market is expensive—over $2.6 billion per drug on average—and takes more than a decade. Clinical Research Informatics helps cut this time and cost by:
Automating data collection and reporting.
Enhancing patient recruitment through AI-driven eligibility matching.
Reducing errors through real-time monitoring and digital audits.
This means that life-saving treatments can reach patients faster, improving healthcare outcomes globally.
6. Regulatory Compliance and Data Security
Clinical trials must adhere to strict regulations from agencies like the FDA, EMA, and ICH-GCP. Informatics ensures that all research data is:
Securely stored and encrypted.
Auditable and traceable, reducing the risk of fraud.
Compliant with regulations, avoiding costly penalties.
This is especially important in an era where cybersecurity threats pose significant risks to patient data. Blockchain technology is also being explored in Clinical Research Informatics to create tamper-proof, transparent data records.
The Google Maps Analogy: How CRI Navigates Clinical Trials
Imagine you’re on a road trip. Without GPS, you rely on old maps, word-of-mouth directions, and trial-and-error driving. This is traditional clinical research—slow, inefficient, and full of uncertainties.
Now, imagine using Google Maps or Waze:
You get real-time traffic updates (real-time patient data).
It suggests faster routes (AI-driven trial optimization).
It warns about roadblocks ahead (predictive analytics for potential failures).
Clinical Research Informatics functions exactly like this for clinical trials, ensuring that researchers take the best, fastest, and safest route to groundbreaking medical discoveries.
Why Clinical Research Informatics is More Relevant Than Ever in 2025?
The world of clinical research is undergoing a massive transformation, driven by technological advancements, regulatory changes, and the increasing demand for faster, more efficient drug development. Clinical Research Informatics (CRI) has emerged as the backbone of modern clinical trials, enabling researchers to harness big data, AI-driven analytics, and real-world evidence (RWE) to improve the success rate of new medical treatments.
Let’s dive deeper into the reasons why Clinical Research Informatics is more crucial than ever in 2025 and how it is reshaping the future of healthcare.
1. The Global Clinical Trials Market is Surging
Clinical research is a booming industry, with the global clinical trials market projected to exceed $80 billion by 2026. This growth is driven by:
The increasing prevalence of chronic diseases.
The need for faster and more cost-effective drug development.
The expansion of precision medicine and personalized treatments.
However, with more trials being conducted worldwide, the industry faces significant challenges:
Rising costs of clinical research.
Patient recruitment and retention issues.
Regulatory hurdles and compliance complexities.
How Clinical Research Informatics Solves This?
Clinical Research Informatics plays a key role in tackling these challenges by:
Automating data management, reducing human error and inefficiencies.
Utilizing predictive analytics to design smarter trials.
Enhancing patient recruitment through AI-driven eligibility screening.
Integrating real-world data (RWD) to make trials more representative and efficient.
By leveraging informatics, researchers can cut trial costs, accelerate timelines, and improve overall success rates—a critical advantage in a highly competitive industry.
2. AI-Driven Analytics Are Reducing Trial Failures by 30%
One of the biggest problems in clinical research is trial failure, which results in billions of dollars in lost investments. In 2025, AI and machine learning are playing an increasingly vital role in reducing trial failures by up to 30% by:
Identifying the right patient populations through AI-driven data analysis.
Predicting potential adverse effects before they happen.
Enhancing study design through real-time data simulations.
Reducing protocol deviations, which are a leading cause of trial delays and failures.
3. Decentralized Clinical Trials (DCTs) Are Reshaping Research
The traditional clinical trial model is logistically complex, expensive, and geographically limited. Decentralized Clinical Trials (DCTs) are changing this by allowing patients to participate from home using:
Wearable devices (e.g., Apple Watch, Fitbit) to collect real-time health data.
Mobile apps and telemedicine for remote consultations and monitoring.
AI-powered patient recruitment platforms that target the right participants faster.
How Clinical Research Informatics Powers DCTs?
CRI provides the digital infrastructure needed for decentralized trials to succeed by:
Securely integrating patient data from multiple remote sources.
Providing real-time data analytics to monitor trial progress.
Ensuring regulatory compliance with digital tracking and auditing tools.
4. Regulatory Agencies Are Pushing for Real-World Evidence (RWE)
Regulatory bodies like the FDA, EMA, and ICH-GCP are increasingly requiring Real-World Evidence (RWE) to support clinical trial data. Unlike traditional trial data, which is collected under controlled environments, RWE is derived from real-life patient experiences and includes:
Electronic Health Records (EHRs).
Insurance claims and billing data.
Patient-generated data from mobile health devices.
Social determinants of health (SDOH), which impact treatment outcomes.
Why This Matters?
RWE enhances drug safety monitoring by identifying rare side effects post-approval.
It speeds up regulatory approvals, making new treatments available faster.
It allows for continuous evaluation of treatments in real-world settings.
Conclusion
Clinical Research Informatics is the future of medicine, and staying ahead means gaining the right expertise. If you’re looking to master this field, CCRPS provides top-tier training to get you industry-ready. Whether you're starting out or upskilling, CCRPS has the resources to make you a leader in Clinical Research Informatics!
Explore Courses for Clinical Research Career
Courses Available:
Frequently Asked Questions (FAQs)
-
The goal is to leverage data and technology to improve the efficiency, quality, and safety of clinical trials.
-
It allows real-time monitoring, reducing adverse events and ensuring early detection of risks.
-
Big data, AI, cloud computing, blockchain, and real-world evidence (RWE) analysis.
-
It reduces trial costs, shortens research timelines, and helps identify successful treatments faster.
-
No! It’s used in hospitals, academia, biotech startups, and regulatory agencies.
-
AI predicts trial outcomes, optimizes recruitment, and automates data analysis.