Top 50 Questions for the Medical Monitor and MSL Certification Exam
Preparing for the dual role of a Medical Monitor and a Medical Science Liaison (MSL) requires more than textbook theory. These roles sit at the intersection of clinical trial oversight and scientific communication, meaning professionals must balance patient safety, regulatory compliance, and real-world stakeholder engagement. Certification validates that balance, proving you can manage adverse events while also driving credible scientific dialogue with investigators and key opinion leaders.
This guide compiles the top 50 exam questions with expert-backed answers, structured around domains every candidate must master: safety management, KOL engagement, compliance, and cross-functional trial responsibilities. Each question is designed to test how well you connect theory to execution. Whether your goal is passing the certification or proving expertise to sponsors, these practice questions are your most direct path to exam mastery.
Why Practice Questions Are the Fastest Way to Master Both Roles
How the Brain Learns Under Test Conditions
Exam prep is most effective when it mirrors real conditions. Cognitive research shows that active recall outperforms passive reading because the brain encodes information more deeply under pressure. By practicing with realistic Medical Monitor and MSL exam questions, candidates strengthen neural pathways tied to problem-solving and pattern recognition. This is critical when interpreting protocol deviations, identifying safety signals, or communicating scientific data.
Simulated test conditions also train time management. Candidates learn to quickly interpret complex scenarios, eliminating distractions and focusing on regulatory priorities. Practicing under these conditions builds endurance, allowing you to stay sharp across long exam sessions. The brain becomes conditioned to retrieve relevant frameworks in seconds, replicating the decision-making speed required in real-world monitoring and liaison work.
How Repeated Exposure Builds Confidence
Success in the Medical Monitor and MSL Certification Exam depends on consistent exposure to exam-style material. Each round of practice reinforces recall, reduces hesitation, and exposes weak points. By reviewing clinical safety scenarios or KOL communication dilemmas repeatedly, candidates can close gaps before exam day. Repetition transforms uncertainty into automatic responses, ensuring accuracy under pressure.
Confidence is not built from theory alone but from applying that theory in multiple contexts. When you’ve answered dozens of SAE handling or compliance-driven questions, the exam feels less like a hurdle and more like a familiar environment. This confidence extends beyond the test—professionals who train with repeated Q&A are better equipped to handle unexpected challenges during clinical trials or scientific discussions, because they’ve already rehearsed problem-solving in structured ways.
Top 50 Medical Monitor & MSL Exam Questions with Expert Answers
| # | Question | Expert Answer |
|---|---|---|
| 1 | What should a Medical Monitor do when a patient reports chest pain during a trial? | Immediately assess seriousness, confirm investigator documentation, and ensure expedited SAE reporting. Consult cardiology experts, evaluate protocol adjustments, and escalate findings to sponsor and IRB. Patient safety takes priority, and consistent communication ensures compliance. |
| 2 | How should incomplete patient data be handled during interim analysis? | Request clarifications from sites, reconcile with CRF data, and document missing information. Apply Good Clinical Practice standards, retrain staff, and implement corrective plans. Complete, accurate data safeguards regulatory credibility and statistical power. |
| 3 | What signals justify a mid-trial protocol amendment? | High deviation rates, unexpected adverse event clusters, or unachievable eligibility criteria. Risk–benefit reassessment and sponsor consultation determine amendments. IRB and regulatory approvals must precede changes to maintain compliance. |
| 4 | What are the top priorities when reviewing site monitoring reports? | Focus on SAE reporting timeliness, informed consent accuracy, and CRF–source data consistency. Address protocol deviations quickly with CAPA. Proper oversight ensures readiness for audits and protects trial integrity. |
| 5 | How can high dropout rates be managed? | Analyze withdrawal reasons, balance patient safety with retention strategies, and implement retraining or protocol adjustments. Escalate findings transparently to sponsors and ethics committees to ensure corrective measures are in place. |
| 6 | How should data discrepancies between CRF and source be resolved? | Initiate queries, review audit trails, and retrain staff. Persistent issues require escalation and possible audits. Data accuracy is non-negotiable for regulatory approval and scientific reliability. |
| 7 | What steps should be taken if safety signals emerge across multiple trials? | Aggregate data, assess biological plausibility, and escalate through safety committees. Initiate risk mitigation strategies and protocol revisions while ensuring consistent site communication and expedited regulatory reporting. |
| 8 | How should data be handled after a patient withdraws consent? | Stop future collection but retain prior data per informed consent laws. Document withdrawal date, ensure privacy compliance, and clarify permissible procedures with regulators and IRBs. |
| 9 | How should SAE causality assessments be validated? | Review history, timing, and alternative causes. Apply objective causality criteria and consult independent experts if needed. Document rationale and ensure regulatory transparency. |
| 10 | How do you maintain data quality in long-term trials? | Implement Quality by Design, centralized monitoring, and regular audits. Train staff continuously and reconcile safety with clinical databases for consistent, reliable data over years. |
| 11 | What defines a Serious Adverse Event and its reporting timeline? | A Serious Adverse Event involves death, hospitalization, disability, or medical importance. Sites report within 24 hours; sponsors report within mandated 7 or 15 days depending on severity. |
| 12 | How do you identify a SUSAR? | A SUSAR is serious, unexpected, and drug-related. Validate against reference safety info, confirm criteria, and expedite reporting within mandated timelines. |
| 13 | When is emergency unblinding justified? | Unblind only if needed for patient safety. Document justification, limit disclosure, and report to sponsor, IRB, and regulators promptly. |
| 14 | How do deviations differ from violations? | A deviation is a minor departure; a violation impacts patient rights or data. Conduct CAPA, retrain staff, and escalate serious issues to oversight bodies. |
| 15 | How should multiple SAEs in one day be prioritized? | Use triage: address life-threatening SAEs first, ensure expedited reporting, and coordinate across safety and clinical teams to avoid backlogs. |
| 16 | How are protocol deviations documented? | Record deviation type, impact on safety and data, and corrective measures. Persistent trends trigger audits and retraining programs. |
| 17 | What corrective actions address frequent dosing errors? | Re-train staff, revise SOPs, and update dosing tools. Prevent recurrence through CAPA and site performance monitoring. |
| 18 | How do you prevent missed SAE deadlines? | Use electronic alerts, 24-hour reporting SOPs, and site training. Regular audits catch delays early and reinforce compliance culture. |
| 19 | How are repeat protocol violations managed? | Escalate to sponsor, suspend enrollment if needed, and enforce CAPA. Protect data credibility by tracking violations across sites. |
| 20 | How do you handle investigator noncompliance? | Engage directly, document noncompliance, implement remediation plans, and escalate if unresolved. Regulatory communication may be necessary. |
| 21 | What is the MSL’s primary role with KOLs? | Provide unbiased, scientific communication, respond to inquiries, and build credibility through data-driven discussions without promotional intent. |
| 22 | How should complex trial data be presented to KOLs? | Translate findings into clear visuals, contextualize clinical impact, and maintain scientific accuracy while avoiding promotional bias. |
| 23 | How do you handle unsolicited off-label questions? | Provide evidence-based non-promotional responses, reference published literature, and document the exchange per compliance policies. |
| 24 | What builds strong KOL relationships? | Consistency, timely responses, and transparent sharing of scientific insights foster trust and credibility long-term. |
| 25 | How should an MSL support investigator-initiated studies? | Guide on feasibility, align with regulatory standards, and provide scientific materials without influencing design or outcomes. |
| 26 | How do MSLs communicate safety updates? | Deliver clear summaries, emphasize patient safety, and ensure consistent messaging across sites while complying with SOPs. |
| 27 | How do you ensure fair balance in data communication? | Present both risks and benefits, cite peer-reviewed evidence, and avoid selective interpretation to maintain trust. |
| 28 | What compliance rules guide slide decks? | Ensure scientific accuracy, use fair balance, and gain medical or legal review before external presentations. |
| 29 | How do you adapt communication for different stakeholders? | Adjust complexity: clinicians need detailed clinical data, while payers need cost-effectiveness evidence, always with accuracy. |
| 30 | How do you measure engagement success? | Track scientific exchange frequency, responsiveness, and feedback quality; focus on knowledge transfer, not sales metrics. |
| 31 | Why is compliance critical in medical affairs? | It ensures patient trust, regulatory alignment, and protects company reputation. Noncompliance risks fines and credibility loss. |
| 32 | How should conflicts of interest be disclosed? | Proactively declare to sponsors, document, and follow transparency policies to maintain integrity in engagements. |
| 33 | What is the MSL’s responsibility in promotional pressure? | Maintain strict non-promotional stance, focusing only on evidence-based, compliant interactions with stakeholders. |
| 34 | How to ensure fair market engagement? | Adhere to local regulations, avoid inducements, and engage only in scientific, not promotional, exchanges. |
| 35 | How are patient privacy laws upheld? | Follow HIPAA and GDPR rules, de-identify data, and secure storage. Privacy breaches can invalidate trial credibility. |
| 36 | What should be done if misconduct is suspected? | Document concerns, escalate to compliance, and ensure audit investigation. Transparency is critical to protect data. |
| 37 | How do you handle undue influence from sponsors? | Resist non-compliant pressure, maintain independent judgment, and document all interactions for compliance audits. |
| 38 | What ethical principles guide KOL interactions? | Respect autonomy, transparency, and evidence integrity; ensure equal treatment across stakeholders. |
| 39 | How are adverse event reports ethically managed? | Report all events, even if uncertain, prioritize patient safety, and maintain clear records for regulators. |
| 40 | What are the consequences of ethical breaches? | Breaches result in regulatory action, trial suspension, and loss of professional credibility for the organization. |
| 41 | What role does a Medical Monitor play in trial design? | Ensure safety endpoints are feasible, protocols align with GCP, and risks are minimized during planning stages. |
| 42 | Why is randomization critical? | It eliminates bias, balances patient factors, and strengthens statistical validity of trial outcomes. |
| 43 | How do you evaluate feasibility of study procedures? | Assess site capacity, patient burden, and resource availability to prevent dropout and protocol deviations. |
| 44 | What defines a robust endpoint? | Endpoints must be clinically relevant, measurable, and reproducible across global sites to support approval. |
| 45 | How are interim analyses safeguarded? | Independent Data Monitoring Committees oversee interim safety and efficacy to prevent premature bias. |
| 46 | How do cross-functional teams support trials? | Collaboration ensures safety oversight, regulatory compliance, and efficient operational execution across sites. |
| 47 | What’s the importance of trial phase knowledge? | Understanding Phase I–IV differences allows tailored monitoring, safety, and communication strategies per stage. |
| 48 | How should protocol amendments be managed? | Submit to regulators and IRBs, re-consent patients, and document changes comprehensively before implementation. |
| 49 | How is trial risk assessed? | Use risk-based monitoring tools, identify critical data points, and apply mitigation strategies to protect integrity. |
| 50 | Why are cross-functional communications vital? | They align medical, regulatory, and operations, ensuring consistent decisions and efficient trial conduct across geographies. |
How to Use These Questions in Your Study Strategy
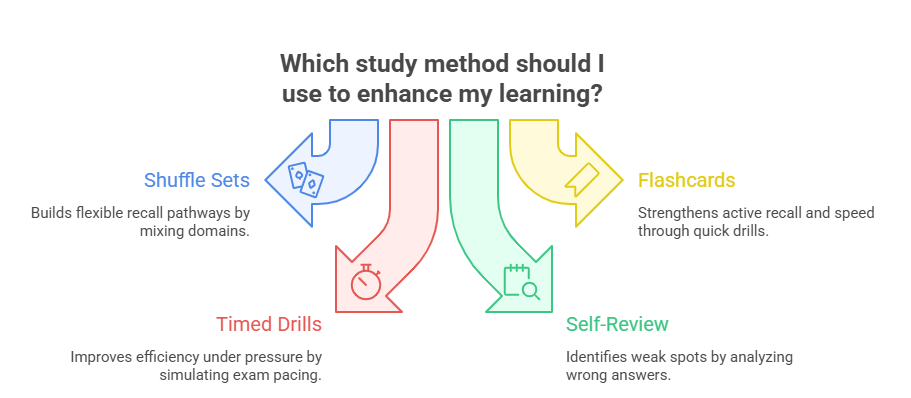
Shuffle Sets for Random Recall Training
One of the fastest ways to master recall is to shuffle question sets regularly. Randomization forces the brain to retrieve knowledge without relying on predictable patterns. By mixing clinical safety, protocol deviation, and KOL engagement questions, candidates replicate the unpredictable nature of the Medical Monitor and MSL Certification Exam. This strengthens retrieval under pressure and highlights weak spots. Building a habit of answering in mixed order helps create flexible knowledge pathways—essential when a real exam or trial situation demands immediate, unbiased judgment.
Combine Questions with Flashcards for Self-Testing
Flashcards remain a proven learning tool when combined with detailed practice questions. Digital or physical formats can both work, but the principle is the same: test yourself frequently, not passively review. Convert Q&A content into flashcards that emphasize core regulatory definitions, SAE criteria, or KOL communication standards. Flashcards enhance active recall, making information retrieval faster and more reliable. Pairing full-length practice questions with flashcards ensures both depth and speed. The result is a sharper ability to answer scenario-based questions quickly while reinforcing critical terminology and regulatory timelines.
Time Yourself Like the Real Exam
Many candidates underestimate timing. The certification exam is strict, and pacing mistakes can derail an otherwise strong performance. To avoid this, practice completing full sets of questions under realistic time limits. Simulate the exam’s pacing rules—allocate no more than one to two minutes per question. Use a timer to reinforce discipline, and review your accuracy afterward. This builds confidence, reduces anxiety, and ensures your responses remain concise and precise. Timed drills train your ability to perform under exam conditions, ensuring you can deliver quality answers within the required constraints.
Avoiding the Most Common Mistakes in MSL & Medical Monitor Exams
Memorizing Instead of Understanding
A major pitfall for candidates is relying on rote memorization. The Medical Monitor and MSL Certification Exam is designed to test application, not recall. Memorizing definitions of SAEs or ICH-GCP terms is insufficient when faced with real-life case studies. For example, identifying whether a liver enzyme spike requires expedited reporting involves contextual judgment, not reciting thresholds. To overcome this, candidates should focus on case-based practice, analyzing patterns, and developing reasoning frameworks. Understanding why a decision is correct strengthens adaptability. This prevents failure when the exam introduces nuanced scenarios or when regulators test deeper knowledge during inspections.
Underestimating Clinical Context Questions
Another frequent mistake is neglecting clinical context. Many candidates excel at compliance or communication definitions but stumble on scenario-driven questions. The exam often embeds subtle clinical variables—comorbidities, concomitant medications, or trial phase considerations—that dramatically change the correct response. Overlooking these leads to errors even if general knowledge is strong. The solution is to consistently practice with scenario-based questions, dissecting each clinical clue before answering. Candidates must learn to integrate safety oversight, communication skills, and compliance into a single decision-making process. Mastering these layered scenarios is essential to passing and thriving as a certified Medical Monitor or MSL.
| Mistake | Description | Better Approach |
|---|---|---|
| Memorizing Instead of Understanding | Candidates rely on rote definitions without applying them to real SAE or compliance scenarios. | Focus on case-based practice, analyze why an answer is correct, and build reasoning frameworks for application. |
| Underestimating Clinical Context Questions | Ignoring patient comorbidities, concomitant medications, or trial phase factors that change the correct decision. | Practice scenario-driven Q&As, dissect each clinical clue, and integrate safety, compliance, and communication into answers. |
Why the CCRPS Medical Monitor & MSL Certification Is the Right Fit
The CCRPS Medical Monitor and MSL Certification is built to prepare professionals for real-world responsibilities. Unlike generic programs, it emphasizes practical decision-making across safety monitoring, protocol oversight, and scientific communication. The curriculum integrates regulatory updates, case-based training, and a robust Q-bank, ensuring candidates are prepared for the exam and daily challenges in medical affairs. This direct alignment between study materials and real scenarios makes CCRPS the most effective choice for advancing a career in clinical research and medical liaison roles.
Real-World Clinical Scenarios
CCRPS’s certification program is structured around real clinical trial situations. Instead of passive theory, candidates work through scenarios on SAE triage, protocol deviations, and investigator queries. This method mirrors the Medical Monitor role, where daily oversight requires quick, evidence-based decisions. By mastering practical applications, candidates gain confidence not only for exam performance but also for real trial environments where regulatory deadlines and patient safety cannot be compromised.
Expert-Driven Scientific Communication Training
For aspiring MSLs, communication with Key Opinion Leaders (KOLs) is a central skill. CCRPS incorporates modules designed by experienced industry professionals who have managed KOL engagement across global markets. Candidates learn how to present trial data effectively, respond to unsolicited questions, and maintain compliance with strict promotional boundaries. This training prepares graduates to represent sponsors with credibility, building trust through accurate and transparent dialogue. The MSL function becomes a true extension of scientific expertise rather than a marketing channel.
Integrated Compliance and Ethics Modules
Regulatory compliance is a recurring exam theme and an everyday professional responsibility. CCRPS ensures candidates are fully trained on global regulations, from ICH-GCP guidelines to region-specific requirements like FDA, EMA, and PMDA expectations. The certification also embeds modules on ethics, ensuring candidates are prepared to handle conflicts of interest, protect patient privacy, and maintain transparency in medical affairs. By grounding learning in compliance, CCRPS equips professionals with the knowledge to avoid costly errors and safeguard trial credibility.
Updated Question Bank and Exam Simulation
A standout feature of CCRPS is its continually updated Q-bank. Candidates gain access to hundreds of practice questions reflecting the most current exam formats. These practice sets include scenario-driven items across safety oversight, trial phases, KOL communication, and compliance risks. Timed simulations help students build exam endurance and develop pacing strategies. With this resource, graduates are not blindsided by new question types and can enter the exam with confidence.
Career Advancement and Industry Recognition
Certification through CCRPS is widely recognized by sponsors, CROs, and regulatory bodies. Graduates demonstrate mastery of both Medical Monitoring and MSL functions, making them highly competitive for advanced roles in clinical research and medical affairs. The CCRPS credential signals to employers that you possess not only theoretical knowledge but also applied expertise. For professionals aiming to move from mid-level positions into leadership, this certification delivers the credibility and skill set necessary for advancement.
Frequently Asked Questions
-
A Medical Monitor oversees clinical trials, ensuring patient safety, protocol compliance, and accurate data reporting. They interact closely with investigators, review adverse events, and guide corrective actions during studies. In contrast, a Medical Science Liaison serves as a scientific communicator between sponsors and healthcare professionals. MSLs focus on engaging Key Opinion Leaders (KOLs), explaining trial data, and supporting investigator-initiated studies. Both roles are vital: one ensures trial integrity, while the other ensures scientific credibility. The Medical Monitor and MSL Certification equips professionals to handle both, creating dual-skilled experts who can pivot across clinical operations and medical affairs with authority.
-
The exam is challenging because it emphasizes applied knowledge rather than rote memorization. Candidates must interpret SAE scenarios, evaluate compliance risks, and respond to case-based questions on scientific communication. Unlike multiple-choice exams testing only definitions, this exam tests judgment under clinical context. Success requires consistent practice with realistic Q&A sets, time management drills, and flashcard-based recall. The updated CCRPS question bank mirrors the latest exam patterns, ensuring familiarity. With structured preparaon, the exam is tough but fair, designed to validate professional readiness. Candidates who engage deeply with case-based materials typically achieve stronger outcomes and career confidence.
-
Preparation timelines vary, but most candidates require two to three months of focused study. Professionals with prior experience in clinical research or medical affairs may progress faster, while newcomers may need extra time. A structured plan combining daily practice questions, review of SAE criteria, and simulated exam drills is essential. Many candidates dedicate 8–10 hours weekly, balancing study with professional responsibilities. The CCRPS certification program provides a guided curriculum, updated Q-bank, and timed simulations, allowing candidates to optimize preparation within a predictable schedule. Commitment and consistency, rather than duration alone, determine exam success.
-
Graduates often step into higher-level roles such as Clinical Trial Medical Monitor, Global Medical Affairs Associate, or Regional Medical Science Liaison. The certification demonstrates mastery across both safety oversight and scientific engagement, making candidates valuable to sponsors, CROs, and biopharma firms. Employers recognize the CCRPS credential as evidence of applied expertise, not just theory. Certified professionals are more likely to be considered for leadership-track roles, protocol design advisory positions, or global MSL networks. In a competitive hiring landscape, this dual certification accelerates career growth by broadening both regulatory credibility and cross-functional collaboration skills.
-
Unlike GCP courses or general research certifications, the Medical Monitor and MSL Certification is role-specific and dual-focused. It integrates safety management, compliance oversight, and KOL communication into one structured exam. Candidates face case studies simulating SAE triage, trial amendments, and scientific dialogue. This format mirrors real job demands, unlike broader certifications that emphasize theory. CCRPS designed the program to provide immediate workplace relevance. While GCP knowledge is necessary, it is insufficient for these roles without applied training. This exam ensures professionals are not only compliant but also capable of real-world decision-making in fast-paced clinical environments.
-
The program covers four integrated areas: safety monitoring, scientific communication, compliance and ethics, and cross-functional trial management. Each area is reinforced with practical scenarios, downloadable resources, and access to a continually updated question bank. Candidates also receive exam simulations that build endurance and confidence. Expert-led modules provide insights into both the Medical Monitor’s oversight responsibilities and the MSL’s KOL engagement strategies. The training is online, flexible, and designed to fit professional schedules. Importantly, CCRPS updates its curriculum regularly to reflect evolving regulations and sponsor expectations, ensuring graduates remain current in industry standards.
Final Thoughts
The path to becoming a certified Medical Monitor or MSL requires more than academic study. Success comes from mastering scenario-based thinking, applying regulatory knowledge under pressure, and communicating science with precision. The Medical Monitor and MSL Certification Exam is intentionally demanding because it mirrors real-world responsibilities where patient safety and trial credibility depend on every decision.
By practicing with structured questions, avoiding memorization traps, and learning from real clinical cases, candidates transform knowledge into actionable expertise. The CCRPS program provides the updated resources, Q-bank, and expert-led training that align preparation with daily professional demands. For those committed to advancing in clinical research or medical affairs, this certification delivers both credibility and confidence to thrive globally.