What is Clinical Trial Management? A Beginner's Guide
Clinical trials are a cornerstone of modern medicine, helping researchers test the safety and efficacy of new drugs, medical devices, and treatment protocols. However, the process of conducting clinical trials is complex and requires meticulous management to ensure successful outcomes. This is where Clinical Trial Management (CTM) comes in. Clinical Trial Management involves overseeing the planning, execution, and monitoring of clinical trials to ensure they are conducted efficiently, ethically, and in compliance with all regulatory requirements.
In this beginner's guide, we’ll explore the key components of clinical trials and the critical role of Clinical Trial Management. From the initial study design to the final data collection, CTM ensures that clinical trials run smoothly, ultimately advancing medical science and patient care.
What Are Clinical Trials and Why Are They Important?
Clinical trials are research studies conducted to evaluate new treatments, therapies, or interventions in humans. These trials are designed to assess how well a new treatment works, how safe it is, and whether it can be more effective than current therapies. Clinical trials provide valuable data that help determine the medical benefits, risks, and overall effectiveness of new treatments.
The importance of clinical trials cannot be overstated. They are the gateway through which new medicines and devices must pass before becoming widely available to the public. Clinical trials ensure that new treatments are safe, effective, and appropriate for the population they are intended to serve. Additionally, clinical trials provide critical insights into the best practices for treating various conditions, ultimately improving healthcare outcomes and patient quality of life.
Key Points:
Safety and Efficacy: Clinical trials help determine if new treatments are safe and effective.
Advancing Science: They are essential for developing new treatments and improving existing ones.
Regulatory Approval: Clinical trials are required by regulatory bodies like the FDA for new drugs and devices to be approved.
What is Clinical Trial Management (CTM)?
Clinical Trial Management (CTM) is the process of overseeing all aspects of a clinical trial from its initiation to its completion. It involves a range of activities, from planning the trial to ensuring that it adheres to regulatory requirements and ethical standards. The main goal of CTM is to ensure that clinical trials are conducted efficiently, within budget, on time, and in compliance with local and international regulations.
Effective Clinical Trial Management is critical for ensuring that a clinical trial produces accurate, reliable results and is conducted with the utmost respect for participants' safety. CTM involves coordinating multiple stakeholders, managing resources, overseeing timelines, and ensuring proper documentation throughout the entire trial process.
Key Functions of Clinical Trial Management:
Study Design: Developing a robust and scientifically sound protocol.
Recruitment: Ensuring that suitable participants are enrolled.
Regulatory Compliance: Meeting ethical standards and complying with regulations.
Data Collection: Gathering, storing, and analyzing trial data efficiently.
CTM is also crucial for minimizing the risk of errors, delays, or regulatory issues that could compromise the trial's outcome or integrity. By maintaining stringent control over all aspects of the trial, CTM professionals help ensure that the results can be trusted and used to make informed decisions.
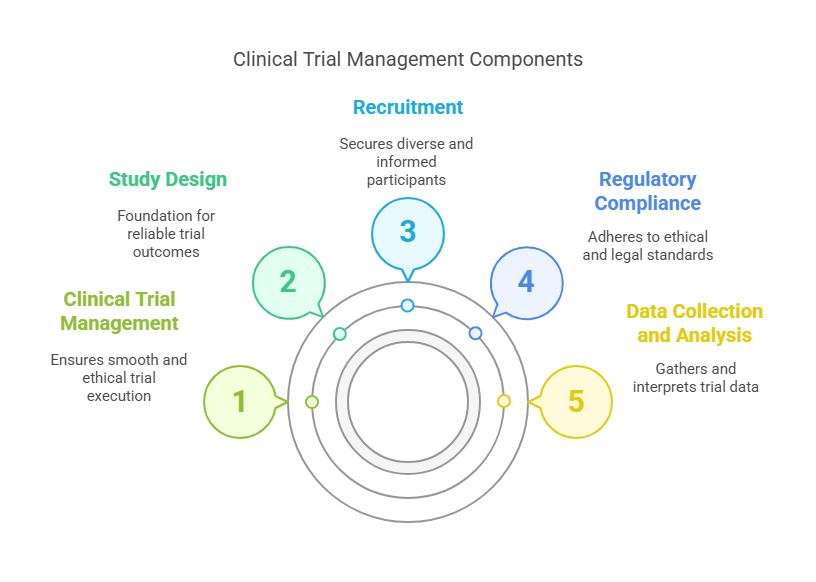
Key Components of Clinical Trial Management (CTM)
To ensure that clinical trials run smoothly, CTM focuses on several key components. Let’s take a closer look at each of them:
1. Study Design
Study design is the foundation of any clinical trial. It outlines the objectives, methodology, and procedures for conducting the trial. A well-designed study ensures that the research questions are clear and the methods will yield reliable and reproducible results. Study design also includes determining the sample size, the selection of appropriate controls, and the use of randomization techniques to minimize bias.
The protocol is the blueprint for the entire study, providing clear instructions on how the trial will be conducted. This document is reviewed and approved by ethical committees and regulatory bodies before the trial can begin.
Key Elements of Study Design:
Trial objectives and endpoints
Randomization and control groups
Inclusion and exclusion criteria
Statistical analysis plan
2. Recruitment
Recruitment involves finding eligible participants who meet the criteria outlined in the study protocol. Recruiting the right participants is crucial for the trial’s success. The recruitment process can involve advertising, working with healthcare providers, and using databases to identify potential candidates.
It's important to ensure that participants are fully informed about the trial and their rights. This is where informed consent comes into play — participants must voluntarily agree to take part in the study after understanding the risks and benefits.
Challenges in Recruitment:
Diverse Participant Pool: Trials often need participants with specific characteristics or conditions.
Ethical Considerations: Ensuring that participants are fully informed and that their participation is voluntary.
3. Regulatory Compliance
Clinical trials are subject to a wide range of regulations and ethical guidelines. Regulatory compliance is an essential part of CTM, ensuring that the trial adheres to all local and international laws, including those set by the FDA, EMA, and ICH-GCP (International Council for Harmonisation – Good Clinical Practice).
Compliance involves ensuring that the trial meets ethical standards, that adverse events are reported promptly, and that the trial's integrity is upheld throughout its duration. Regular audits and inspections by regulatory authorities are common to ensure compliance is maintained.
Key Regulatory Bodies:
FDA (Food and Drug Administration): U.S. regulatory authority for clinical trials involving drugs and devices.
EMA (European Medicines Agency): Oversees clinical trials in the European Union.
ICH-GCP: Provides global guidelines for conducting clinical trials ethically.
4. Data Collection and Analysis
Data collection is a crucial aspect of any clinical trial. Accurate and consistent data is necessary to determine whether the trial's treatment is effective and safe. Data is typically gathered through clinical visits, laboratory tests, surveys, and medical evaluations.
The data must be analyzed according to the pre-established statistical analysis plan, which outlines how the results will be interpreted. Data integrity is paramount, and the use of Electronic Data Capture (EDC) systems ensures that the data is stored securely and is accessible for analysis and reporting.
Challenges in Data Management:
Quality Control: Ensuring data is accurate, complete, and reliable.
Data Security: Protecting patient confidentiality and preventing data breaches.
Who Is Involved in Clinical Trial Management?
Clinical Trial Management involves a variety of professionals who work together to ensure the trial is conducted properly. Some of the key roles in CTM include:
1. Project Managers
Clinical trial project managers oversee the entire trial process. They are responsible for planning the trial, coordinating with team members, ensuring timelines are met, and managing budgets. They ensure that all aspects of the trial are completed according to the protocol and in compliance with regulations.
2. Clinical Researchers
Clinical researchers (often physicians or medical professionals) design the study, conduct patient assessments, and analyze the data. They are integral to ensuring the clinical questions are addressed and that the trial adheres to ethical standards.
3. Clinical Research Coordinators (CRCs)
CRCs are responsible for the day-to-day operations of a clinical trial. They recruit and monitor participants, manage data collection, and ensure that all documentation is accurate and up-to-date.
4. Regulatory Bodies
Regulatory bodies, such as the FDA or EMA, provide oversight for clinical trials. They ensure that trials comply with legal and ethical standards and that patient safety is prioritized.
10 Lesser-Known Facts About Clinical Trials
First clinical trial: The first recorded clinical trial was conducted in 1747 by James Lind, who tested the effects of citrus fruits on sailors suffering from scurvy. (Source)
Placebo effect: Placebo-controlled trials are designed to measure the effect of a treatment compared to a placebo, helping scientists separate actual treatment effects from psychological responses. (Source)
Clinical trial phases: Clinical trials progress through four phases, with Phase 1 focusing on safety and Phase 4 on post-market surveillance. (Source)
Regulatory bodies: The FDA oversees the approval of drugs and devices in the U.S., while the EMA performs the same function for Europe. (Source)
Blinded trials: In blinded trials, participants are unaware of whether they are receiving the treatment or a placebo to avoid bias.
Global recruitment: Some clinical trials include participants from multiple countries to ensure the results are applicable to diverse populations.
Expanded access programs: These programs allow patients to access experimental treatments outside of clinical trials when no other treatment options are available.
Real-world evidence: After a drug is approved, real-world evidence from ongoing trials and post-market studies helps monitor its long-term effects.
Ethics boards: Institutional Review Boards (IRBs) are responsible for reviewing and approving study protocols to ensure that participant safety and rights are protected.
Patient diversity: Clinical trials aim to include a diverse group of participants to ensure that treatments work across different demographics, including age, gender, and ethnicity.
Related Blogs
How Clinical Trials and Data Management Impact Research Outcomes?
The Basics of Clinical Trial Data Management
Conclusion
Clinical Trial Management is crucial for ensuring that clinical trials run efficiently, ethically, and within regulatory guidelines. By overseeing key components such as study design, recruitment, regulatory compliance, and data collection, CTM professionals ensure that clinical trials produce reliable results that contribute to medical advancement. The collaboration of project managers, researchers, coordinators, and regulatory bodies is essential to maintaining the integrity of the trial process.
At CCRPS, we are dedicated to supporting clinical trial success with the highest standards of clinical trial management, ensuring compliance, accuracy, and efficiency in every step of the process.
Frequently Asked Questions (FAQs)
-
Clinical Trial Management ensures that clinical trials are conducted efficiently, on time, and in compliance with all ethical and regulatory requirements. It helps coordinate all aspects of the trial to guarantee reliable results.
-
Clinical trial managers, researchers, coordinators, and regulatory bodies are all responsible for overseeing different aspects of clinical trial management.
-
Regulatory compliance is ensured through adherence to local and international guidelines, regular audits, and maintaining documentation in accordance with standards set by organizations like the FDA and EMA.
-
The key components include study design, participant recruitment, regulatory compliance, and data collection.
-
Data is collected through clinical visits, laboratory tests, and patient surveys. Electronic Data Capture (EDC) systems are often used to ensure data accuracy and security.