Phase II Clinical Trials: Goals, Examples, and Real-Life Insights
Phase II clinical trials are the critical bridge between exploratory Phase I studies and confirmatory Phase III trials. They focus on determining a treatment’s efficacy in specific patient populations while closely monitoring safety and tolerability. Unlike Phase I, which tests general safety in healthy volunteers, Phase II trials measure how well the drug works in those with the targeted condition. This phase narrows down dosages, establishes response benchmarks, and sets the foundation for future protocols. Understanding Phase II’s role is essential for clinical research associates (CRAs), sponsors, and regulators who ensure trial integrity and participant safety.
Real-world insights show that Phase II outcomes directly influence drug development timelines and regulatory pathways. A robust Phase II study provides the data backbone for Phase III, determining whether the treatment will move forward or face significant setbacks. Additionally, Phase II results guide adaptive trial designs, enabling faster pivots in response to preliminary data. These trials offer crucial lessons for professionals aiming to master site management, data monitoring, and protocol compliance. For those pursuing certifications like Advanced Clinical Research Associate Certification, Phase II understanding transforms theoretical knowledge into actionable expertise.
Understanding the Core Goals of Phase II Clinical Trials
Efficacy: Measuring Treatment Impact
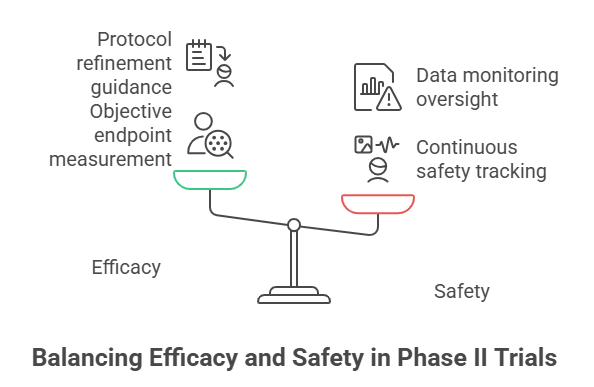
Phase II trials primarily assess treatment efficacy in specific patient populations. Unlike Phase I’s focus on safety, this phase tests whether the investigational drug delivers clinically meaningful results. Researchers measure key response metrics—such as tumor shrinkage in oncology or symptom improvement in autoimmune diseases—using pre-defined, objective endpoints. Clear and quantifiable endpoints reduce ambiguity, ensuring data integrity and comparability across study sites.
For example, oncology trials often employ RECIST criteria, which objectively measure tumor size reductions. In chronic diseases, researchers may use symptom scales or biomarker changes to assess response. Effective endpoint selection is crucial; endpoints that align with regulatory expectations increase the likelihood of success in subsequent phases.
Moreover, efficacy findings can reshape therapeutic protocols, as seen with HER2-targeted treatments or innovative antiviral regimens. Early efficacy signals also enable adaptive design modifications, refining dose regimens or patient stratification. For CRAs and sponsors, recognizing how efficacy endpoints influence trial outcomes fosters proactive decision-making and regulatory alignment.
Safety and Side Effects Profile
While Phase II trials emphasize efficacy, they also provide crucial safety data. Continuous monitoring identifies adverse events (AEs) and serious adverse events (SAEs), often using standardized criteria like CTCAE for consistency. Safety assessments track both common side effects (e.g., gastrointestinal issues) and rare, potentially life-threatening events.
Balancing therapeutic gains against safety risks is a regulatory priority. Sponsors and investigators establish data monitoring committees (DMCs) to oversee ongoing safety profiles, ensuring participant well-being. Real-time data capture, coupled with early stopping rules, mitigates risks if unacceptable toxicity levels emerge.
Additionally, regulatory bodies such as the FDA and EMA expect Phase II trials to provide sufficient safety evidence before allowing progression to Phase III. These agencies scrutinize adverse event patterns, dose-limiting toxicities, and participant-reported outcomes. Trials demonstrating a favorable risk-benefit profile advance faster, while those with safety concerns may face delays or termination.
CRAs must understand these nuances, as monitoring safety endpoints is integral to site management and compliance. Mastery of Phase II safety considerations prepares professionals for roles requiring precise oversight and proactive risk management.
Key Design Elements in Phase II Trials
Randomization and Blinding Approaches
Randomization and blinding reduce bias and strengthen the validity of Phase II trial results. Single-blind designs conceal treatment allocation from participants, while double-blind methods hide it from both participants and investigators. Adaptive trial designs introduce real-time modifications based on interim data, improving efficiency without compromising data integrity. By reducing selection bias and placebo effects, these methods enhance the reliability of efficacy and safety findings.
Implementing effective blinding in multi-center trials ensures consistency across sites. CRAs must verify blinding protocols and monitor adherence to avoid protocol deviations that could compromise trial outcomes. For regulatory approval, documented evidence of robust randomization and blinding is essential.
Sample Size and Statistical Power
Accurate sample size determination ensures statistical significance of trial outcomes. Underpowered studies risk false negatives, while overly large samples may waste resources and expose participants to unnecessary risks. Researchers use power calculations that consider expected effect sizes, variability, and significance thresholds to determine optimal participant numbers.
Common pitfalls include underestimating variability or overestimating treatment effects. Adaptive sample size re-estimation, informed by interim data, can correct these issues mid-trial. CRAs and sponsors must ensure adherence to these calculations to maintain regulatory compliance and protect participant welfare. Proper sample size decisions directly impact a trial’s credibility and progression to Phase III.
Dose Optimization Strategies
Identifying the optimal dose is a central goal of Phase II trials. This involves balancing efficacy with safety to find the dose that offers maximal therapeutic benefit with minimal adverse effects. Pharmacokinetic (PK) and pharmacodynamic (PD) studies inform dose selection, evaluating how the drug behaves in the body and its biological effects.
Dose-escalation protocols, such as modified continual reassessment methods (mCRM), adjust doses based on real-time safety and efficacy data. Incorporating adaptive dose modifications ensures participant safety while refining dosing strategies for future trials. CRAs must track dose changes accurately and ensure that investigator sites implement adjustments consistently. These strategies help define the optimal dose for Phase III, improving trial success rates.
| Key Design Elements | Description |
|---|---|
| Randomization and Blinding Approaches | Reduces bias and strengthens the validity of Phase II trial data. Includes single-blind, double-blind, and adaptive designs to ensure reliable results. CRAs monitor adherence to blinding protocols, which is crucial for regulatory approval and data integrity. |
| Sample Size and Statistical Power | Ensures trials have enough participants to detect meaningful treatment effects. Power calculations consider effect size, variability, and significance thresholds. Adaptive sample size adjustments are used mid-trial to maintain accuracy and efficiency. CRAs monitor adherence and correct deviations to protect credibility and enable progression to Phase III. |
| Dose Optimization Strategies | Identifies the dose with the best balance of efficacy and safety. Pharmacokinetic (PK) and pharmacodynamic (PD) studies guide selection, while dose-escalation protocols and adaptive modifications adjust dosing based on real-time data. CRAs ensure accurate dose changes, documentation, and consistent site implementation. |
Real-Life Phase II Clinical Trial Examples
Oncology Trials: Pioneering Targeted Therapies
Phase II oncology trials have revolutionized cancer treatment, with therapies like HER2-targeted agents and PD-1/PD-L1 checkpoint inhibitors reshaping clinical protocols. These trials focus on objective response rates, progression-free survival, and biomarker-driven endpoints. For instance, studies on trastuzumab (Herceptin) in HER2-positive breast cancer demonstrated significant tumor shrinkage and improved survival, paving the way for global approval.
Checkpoint inhibitors, such as pembrolizumab and nivolumab, showed promising results in early Phase II trials for melanoma and lung cancer. These studies highlighted the power of targeting immune checkpoints to unlock durable responses. Oncology Phase II trials often employ adaptive designs and biomarker-enriched populations to increase the likelihood of success.
CRAs managing these trials must understand complex inclusion criteria, monitor biomarker collection protocols, and track adverse events meticulously. Precision oncology has set a new benchmark for Phase II trials, requiring robust operational oversight and a deep understanding of molecular pathways.
Infectious Disease Studies: Fast-Tracking Innovation
Phase II trials in infectious diseases exemplify agile trial design during public health crises. The COVID-19 pandemic highlighted this approach, with antiviral agents like remdesivir undergoing rapid Phase II evaluation. These trials balanced speed with safety, employing adaptive protocols and real-time data monitoring to assess viral clearance rates and clinical improvement.
Earlier, HIV research relied on Phase II trials to identify effective antiretroviral combinations. Trials testing combination therapies such as zidovudine and lamivudine revealed significant reductions in viral load, setting the stage for broader treatment protocols. Fast-tracked Phase II trials for Ebola vaccines demonstrated protective immunity in high-risk populations, validating accelerated pathways for urgent threats.
CRAs involved in these studies must manage dynamic enrollment targets, evolving protocols, and complex logistics like cold chain management for biologics. Infectious disease Phase II trials demand precision and adaptability, ensuring that trial integrity is maintained even under crisis conditions.
Challenges and Solutions in Phase II Trials
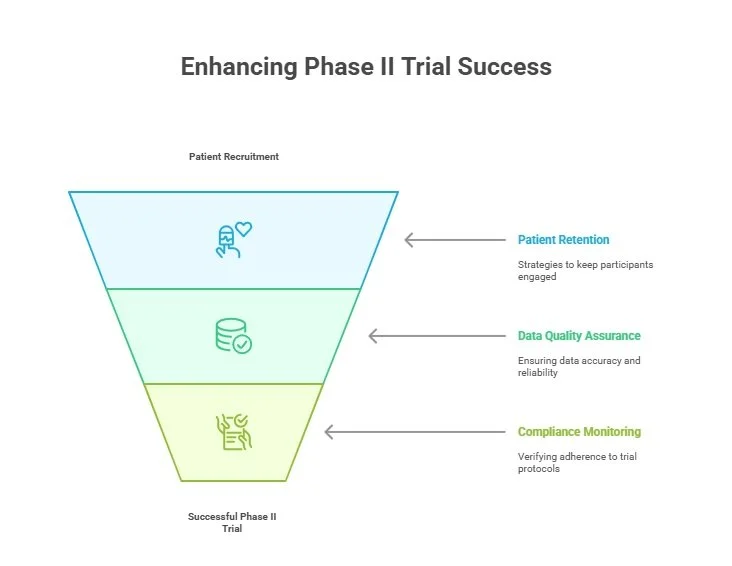
Patient Recruitment and Retention
Recruiting and retaining patients in Phase II trials is a persistent challenge. Delays in enrollment and high dropout rates can jeopardize timelines and data integrity. Common hurdles include limited awareness, logistical barriers, and stringent inclusion criteria that narrow the eligible pool. For rare diseases or niche indications, finding suitable participants becomes even harder.
Strategies to overcome these challenges include leveraging patient advocacy groups, offering travel support, and simplifying visit schedules. Enhanced digital outreach, telemedicine visits, and real-time communication platforms also help. Diverse recruitment efforts improve population representation, which strengthens trial validity and meets regulatory expectations. CRAs play a pivotal role in ensuring sites meet recruitment targets while maintaining participant engagement through proactive monitoring and support.
Data Quality and Compliance Issues
Maintaining data quality and compliance is crucial for Phase II trial success. Common protocol deviations—like missed visits, dosing errors, and incomplete data—can compromise study validity and trigger regulatory actions. Real-time monitoring tools, including electronic data capture (EDC) systems and centralized monitoring dashboards, reduce these risks.
CRAs must verify that all data entries align with source documents and monitor adherence to protocols. Regular site audits and staff training sessions ensure that errors are minimized and resolved swiftly. Implementing corrective action plans for recurring issues enhances compliance. Ultimately, rigorous data quality practices protect trial integrity and pave the way for smooth progression to Phase III.
Regulatory Oversight and Ethical Considerations
ICH-GCP and Regulatory Guidelines
Phase II trials must comply with strict international standards, including ICH-GCP, FDA’s 21 CFR, and EMA directives. These guidelines ensure trial integrity, participant safety, and regulatory acceptance. ICH-GCP outlines best practices for protocol development, data management, and monitoring. U.S. regulations (21 CFR) impose additional controls, requiring accurate reporting, recordkeeping, and oversight.
Regulatory bodies demand robust documentation—ranging from site initiation logs to adverse event reports—to assess trial conduct. Non-compliance can delay approval or lead to trial termination. CRAs ensure that study sites implement protocols correctly, maintain accurate records, and prepare for regulatory inspections. Mastery of ICH-GCP principles is essential for CRAs pursuing certifications like the Advanced Clinical Research Associate Certification, equipping them to navigate complex compliance landscapes confidently.
Informed Consent and Vulnerable Populations
Informed consent is central to ethical trial conduct, requiring clear explanations of risks, benefits, and rights. Participants must have ample opportunity to ask questions and withdraw without penalty. Vulnerable populations—such as children, cognitively impaired individuals, and economically disadvantaged groups—require additional safeguards. These include involving legal representatives, adapting consent forms for literacy levels, and conducting consent discussions in the participant’s preferred language.
Ethics committees and institutional review boards (IRBs) rigorously review informed consent procedures, emphasizing participant autonomy. Failure to implement robust consent processes can result in regulatory sanctions and reputational damage. CRAs must oversee informed consent processes, ensuring documentation is complete and protocol deviations are promptly addressed. Mastery of ethical considerations enhances trial integrity and fosters public trust.
How Phase II Knowledge Strengthens Your CRA Role
Understanding Phase II clinical trials is crucial for Clinical Research Associates (CRAs) pursuing advanced certifications. The Advanced Clinical Research Associate Certification (CCRPS) emphasizes the skills needed to manage, monitor, and ensure compliance in these complex trials. Knowledge of Phase II trial designs—ranging from adaptive randomization to dose optimization—enables CRAs to proactively identify issues and implement corrective actions, safeguarding data integrity and participant safety.
CRAs play a pivotal role in site management, ensuring adherence to complex protocols that incorporate evolving efficacy and safety data. Phase II trials often involve biomarker-driven designs, necessitating a deep understanding of molecular targets, sample handling, and patient stratification. This certification program equips CRAs with the expertise to monitor such nuanced elements effectively.
Additionally, regulatory compliance is non-negotiable. Phase II trials face rigorous scrutiny from regulatory bodies like the FDA, EMA, and national authorities. The Advanced CRA Certification course integrates ICH-GCP principles, audit preparedness, and real-time problem-solving skills essential for navigating these challenges. CRAs must ensure complete documentation, monitor adverse events, and support sites in meeting strict data quality standards.
Phase II experience also hones skills in patient engagement. CRAs learn to identify and mitigate patient recruitment and retention challenges through targeted communication strategies and logistical support. This proactive approach not only strengthens site relationships but also reduces dropout rates, a critical success factor in Phase II studies.
For those seeking to elevate their CRA careers, the CCRPS Advanced Clinical Research Associate Certification offers unparalleled insights into Phase II trials. Mastery of Phase II concepts enables CRAs to make informed decisions, anticipate regulatory concerns, and support sponsors in achieving trial objectives. To explore how this certification can transform your clinical research career, visit the Advanced CRA Certification page here.
Final Thoughts
Phase II clinical trials represent a pivotal turning point in drug development, shaping the trajectory of treatments and setting the groundwork for large-scale efficacy testing. Their design, execution, and analysis demand rigorous attention to detail, balancing scientific precision with participant safety. The insights gained from Phase II studies not only dictate the advancement of promising therapies but also refine operational strategies that benefit future research.
For clinical research professionals, Phase II knowledge is more than technical proficiency—it’s a strategic asset. Whether managing site operations, ensuring data quality, or safeguarding patient welfare, mastery of this phase empowers professionals to excel in an increasingly complex landscape. Aspiring CRAs, particularly those pursuing the Advanced Clinical Research Associate Certification, will find that Phase II expertise enhances their ability to drive trial success, navigate regulatory requirements, and contribute to meaningful medical innovation.
By embracing the challenges and opportunities of Phase II trials, today’s clinical research professionals position themselves at the forefront of a rapidly evolving industry, advancing both their careers and the future of healthcare.
Frequently Asked Questions
-
Phase II trials focus on evaluating a drug’s efficacy and safety in target patient populations, unlike Phase I, which tests general safety in healthy volunteers, and Phase III, which assesses large-scale effectiveness. Phase II refines dosages, identifies optimal endpoints, and detects early efficacy signals. Results from Phase II directly impact trial progression, regulatory decisions, and study design for Phase III. Its strategic role is crucial for stakeholders seeking robust clinical data to support further development and regulatory approval.
-
Accurate sample size calculations ensure statistical power to detect meaningful treatment effects. Underpowered studies risk false negatives, while oversized samples waste resources and increase participant burden. Researchers use power calculations, considering effect sizes and variability, to determine optimal enrollment. Adaptive re-estimation may adjust numbers based on interim results. CRAs play a key role in monitoring sample sizes and ensuring adherence to calculations. Correct sample sizing boosts trial validity, expedites regulatory review, and protects participant welfare.
-
Phase II trials implement real-time safety monitoring systems to track adverse events (AEs) and serious adverse events (SAEs). Investigators report AEs using standardized criteria like CTCAE, while data monitoring committees review safety data and recommend actions. Protocols include early stopping rules for unacceptable toxicity levels. CRAs ensure accurate AE documentation, support corrective actions, and maintain regulatory compliance. These processes safeguard participant well-being and inform dose adjustments for future trials.
-
CRAs oversee site management, data integrity, and protocol compliance. They monitor patient recruitment, informed consent, adverse events, and data entry to ensure adherence to protocols and regulations. CRAs identify deviations, support corrective actions, and facilitate audit preparedness. Their expertise is vital for maintaining trial integrity, participant safety, and data credibility. Pursuing the Advanced Clinical Research Associate Certification deepens understanding of these roles, enhancing career progression in clinical research.
-
Adaptive designs allow real-time modifications based on interim data, improving trial efficiency without compromising integrity. Adjustments may include dose changes, sample size re-estimation, or patient stratification based on biomarkers. These designs optimize resource use and accelerate decision-making. CRAs and sponsors must implement adaptive protocols meticulously to avoid bias and maintain regulatory compliance. Adaptive designs enhance flexibility and data quality, making Phase II trials more responsive to emerging insights.
-
Informed consent ensures participant autonomy, requiring clear explanations of risks, benefits, and rights. Vulnerable groups—such as children or cognitively impaired individuals—receive extra safeguards like simplified forms and legal representative involvement. IRBs rigorously review consent procedures to uphold ethical standards. CRAs verify proper documentation, conduct site audits, and address deviations promptly. Strong consent protocols foster trust and protect participant welfare, key to ethical Phase II trial conduct.
-
Phase II trials employ electronic data capture (EDC) systems, centralized monitoring dashboards, and real-time analytics to track protocol adherence and data accuracy. These systems flag inconsistencies, enable corrective actions, and reduce risks of non-compliance. CRAs are responsible for overseeing data systems, verifying source documentation, and ensuring seamless communication with sites. High-quality data monitoring safeguards trial integrity and facilitates efficient regulatory review.
-
Biomarkers provide objective indicators of treatment response, improving precision and enhancing patient selection. In oncology, Phase II trials use biomarkers to identify responsive subpopulations, optimize dosing, and track disease progression. Examples include HER2 in breast cancer and PD-L1 in lung cancer. CRAs manage biomarker sample collection, handling, and documentation, ensuring integrity and regulatory compliance. Biomarker integration elevates trial quality, accelerates approvals, and refines targeted therapy strategies.