Clinical Trials Coordinator Career Pathway: Steps, Salaries, and Advancement (2025)
Clinical Trials Coordinators are the operational heartbeat of a study site. When this role is done right, enrollment moves faster, data queries drop, audits feel boring, and sponsors keep sending more work. When it is done wrong, you live in constant fire drills: missed visits, protocol deviations, angry monitors, and a PI who is “too busy” for everything. This 2025 roadmap shows you how to enter the role, build leverage fast, negotiate pay with evidence, and move into higher-paying tracks without getting trapped in low-growth coordinator jobs.
1) What a Clinical Trials Coordinator Actually Does (And Why Most People Get Stuck)
A Clinical Trials Coordinator is not “admin help.” You are a risk manager for human-subject research and a throughput manager for a revenue engine. Your job is to keep participants safe, keep the protocol clean, and keep documentation audit-ready while balancing sponsor expectations, investigator availability, and real-world clinic chaos. If you want fast advancement, you must start treating the role like operations leadership, not task completion.
The core deliverables sponsors and PIs secretly judge you on
Most coordinators think they are judged on “being helpful.” Sponsors do not care. They judge you on outcomes:
Enrollment velocity without sloppy screening. That means fewer screen failures and faster cycle times from referral to consent to randomization.
Deviation control. Not “zero deviations” (unrealistic), but deviations that are identified early, documented cleanly, and prevented from repeating.
Data cleanliness. You are measured by query volume, query aging, and how often your source does not support the eCRF. If you want to become a lead, you must master query management and source-to-EDC alignment using real systems from the top EDC platforms guide.
Regulatory readiness. You do not “do reg.” You protect the site from compliance debt. This is how coordinators pivot into regulatory using the Regulatory Affairs Specialist roadmap and the Clinical Regulatory Specialist pathway.
The hidden pain points that kill coordinator careers
If you want to grow, you must name the real traps:
You become the “everything person.” That feels valuable but it blocks specialization. You need a plan to become “the person who drives X metric,” like recruitment conversion or query closure. Use the patient recruitment companies and tech list to learn what modern sites use and bring solutions.
Your PI is unavailable. That is normal. Advancement comes from building PI-proof workflows: visit prep packets, pre-signed templates, escalation rules, and documented delegation. If you want PI-level credibility later, study the Principal Investigator roadmap and the Sub-Investigator pathway now so you understand what investigators are accountable for.
You are “busy” but not promotable. Busy is not leverage. Promotable means you can run a study with fewer touches, fewer misses, and cleaner evidence. Coordinators who advance learn the systems mindset from adjacent tracks like Clinical Data Manager and Quality Assurance (QA) Specialist.
You do not document your value. If your resume is “scheduled visits, entered data,” you will get lateral offers and small raises. You need proof: enrollment numbers, query aging reductions, deviation reductions, audit outcomes, cycle times, and training leadership. Benchmark yourself against 2025 comp using the Clinical Research Salary Report 2025 and the CRC Salary Guide 2025.
2) 2025 Salaries: What Coordinators Earn and How to Push Into Higher Bands
If you want more pay, you need two things: a realistic market anchor and a credible “why me” story backed by proof. Markets vary, but compensation patterns are consistent: coordinators who can recruit, run complex protocols, and protect compliance earn more and move faster.
Market anchors you can use without sounding naïve
For the US market, pay datasets often place “Clinical Trial Coordinator” around the low $70Ks, with common ranges spanning roughly the high $50Ks through around $90K+ depending on experience and geography. Glassdoor’s US estimate for Clinical Trial Coordinator is about $72K average, with a range that extends upward into higher percentiles. Glassdoor
Indeed’s US hourly estimate for “Clinical Research Coordinator” is about $28/hour, which annualizes near the high $50Ks, with wide variation by location and seniority. Indeed
PayScale’s estimate for “Clinical Trials Coordinator” in 2025 is around $52K average, typically reflecting broader mixes of settings and experience. Payscale
Do not argue “the internet says.” Instead, use CCRPS benchmarks and role-specific context from the CRC Salary Guide 2025 and the Clinical Research Salary Report 2025. Then attach your personal proof.
Why some coordinators get paid more for the same title
Two coordinators can have identical titles and completely different value:
Coordinator A schedules visits and enters data.
Coordinator B raises enrollment, reduces query aging, prevents repeat deviations, and can onboard new studies fast.
Coordinator B becomes a lead, a site manager, or a bridge into higher-paying tracks like Clinical Research Project Manager or QA Specialist. That is the advancement logic: pay follows risk reduction and throughput.
A salary strategy that works even if your site is cheap
If your employer blocks raises, you still build leverage. Use this three-part system:
Track one metric weekly. Pick a metric that management cares about: screen failure rate, consent error rate, query aging, deviation recurrence. Tie it to sponsor happiness. Connect your work to outcomes used in CRO and sponsor environments from the top CRO vendors and solutions list.
Build a portable portfolio. Document workflows you designed: screening scripts, visit prep checklists, source templates, query triage SOPs. That portfolio helps you pivot into roles like Clinical Research Administrator or data paths like Clinical Data Coordinator.
Move laterally to move up. If you cannot get promoted where you are, shift to a growth site: academic centers, high-volume networks, oncology clinics. Use the top academic medical centers list as a target map.
3) Step-by-Step Career Pathway: From “New Coordinator” to Lead and Beyond
Most people fail because they do not have a 12-month map. They just survive. Here is the pathway that creates promotions.
Step 1: Build your foundation in the first 30 days
Your first month is not about learning everything. It is about learning the non-negotiables:
Consent mastery: version control, comprehension checks, documentation discipline.
Source discipline: if it is not documented, it did not happen. This mindset is what later supports QA pivots via the QA Specialist roadmap.
Protocol navigation: learn where the schedule of events drives everything. If you cannot read a protocol like a blueprint, you will always react late.
If exams and credentialing are part of your plan, build a structured approach using proven test-taking strategies and a serious study environment setup guide.
Step 2: Become independently reliable by day 60
Promotion is based on trust. You earn trust by being predictable:
Visits run on time because you prepare: meds, labs, required questionnaires, IP accountability.
Issues are escalated early. You do not hide problems until monitoring day.
Your documentation is retrieval-ready. When monitors ask, you produce evidence quickly.
To move faster, start learning adjacent systems coordinators touch indirectly, like remote monitoring workflows and oversight norms in modern programs. Study the tooling landscape in the remote monitoring tools guide so you understand what sponsors expect.
Step 3: Own a lane by month 3 to month 6
This is the moment most coordinators miss. They keep doing everything. Instead, pick a lane that creates leverage:
Lane A: Recruitment and retention
If you can recruit, you become valuable. Use operational ideas from the patient recruitment mega list. Build referral scripts, follow-up cadences, no-show prevention, and retention touchpoints.
Lane B: Data and query control
Own query aging. Reduce back-and-forth with clean source. If you like this, you are a future Clinical Data Manager or Lead Clinical Data Analyst.
Lane C: Regulatory and documentation control
Own ISF hygiene and approvals. That is a direct bridge into Regulatory Affairs Associate and more advanced regulatory roles.
Step 4: Lead study start-up execution by month 6 to month 12
When you can onboard a new protocol smoothly, you become promotable. A strong coordinator can:
Build study binders and tracker systems fast
Train staff and keep delegation clean
Forecast visit capacity and staffing bottlenecks
Prevent early deviations with process design
That leadership is what later supports a move into broader site operations leadership like Clinical Research Administrator or sponsor-facing tracks like CRA and PM using the CRA salary data report and the Project Manager salary trends guide.
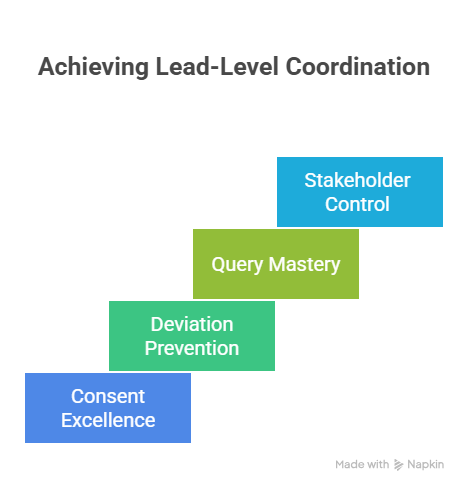
4) The Promotion Skill Stack: What You Must Master to Become “Lead-Level”
You do not become a lead by working harder. You become a lead by reducing uncertainty for everyone else. That requires specific competencies.
A) Consent excellence without shortcuts
Consent mistakes create regulatory risk and destroy sponsor trust. Lead-level coordinators:
Control versioning so old forms never appear in clinic
Train staff on comprehension checks
Document conversations clearly and consistently
Prevent “consent drift” where staff improvise explanations
If your long-term goal is investigator-level work, align your training with the PI accountability mindset using the Principal Investigator roadmap and the Sub-Investigator pathway.
B) Deviation prevention systems
Sites do not fire people for one deviation. They lose contracts because of repeated patterns. Build systems:
Visit-day checklists mapped to schedule of events
Lab kit inventory control and backup plans
IP accountability routines
Clear escalation rules for out-of-window visits
This systems mindset mirrors what QA roles do daily. Study the logic behind prevention and documentation in the QA Specialist roadmap.
C) Query mastery and clean evidence
If you cannot manage queries, you cannot scale. Coordinators who advance treat query aging like revenue leakage:
Triage new queries quickly
Fix root causes in source documentation
Build templates for common recurring issues
Close the loop with training so the same issue does not return
If you enjoy this work, you are a strong candidate for data tracks like Clinical Data Coordinator and eventually Clinical Data Manager. Use the EDC platforms guide to speak the same language as sponsors.
D) Stakeholder control without conflict
A high-performing coordinator can manage tension with calm authority:
Patients want clarity, not confusion
PIs want fewer interruptions, not more meetings
Sponsors want clean data, not explanations
Your job is to make conflicts smaller by preparing earlier, communicating faster, and documenting cleanly. That same stakeholder control is what later supports PM pathways using the Project Manager salary trends guide.
5) Advancement Paths in 2025: Pick a Track That Matches Your Strengths (And Pays)
A coordinator career is not one ladder. It is multiple ladders. The fastest growth happens when you choose based on your strengths and build a portfolio that proves it.
Path 1: Senior Coordinator to Site Manager (operations leadership)
This is the most direct path. You become the person who ensures multiple studies run smoothly. Your resume must show you can scale people and process. From here, you can move into broader leadership roles aligned with Clinical Research Administrator.
Path 2: CRA or remote monitoring direction (sponsor-facing)
If you want travel, cross-site visibility, and sponsor operations exposure, CRA is a common move. This is where your “audit-ready” habits pay off. Use compensation context from the CRA salary report and learn the ecosystem sponsors use from the remote monitoring tools guide.
Path 3: Regulatory affairs specialization (documentation power)
If you love structure, approvals, and precision, regulatory is a high-leverage pivot. Start by owning ISF/TMF hygiene and then align to the Regulatory Affairs Associate guide or the Regulatory Affairs Specialist roadmap. This path often yields more predictable schedules than high-volume coordinator roles.
Path 4: Clinical data management (systems and evidence)
If you find satisfaction in clean evidence and fewer human variables, go data. Build EDC fluency using the top EDC platforms guide, and map your growth toward Clinical Data Coordinator and Lead Clinical Data Analyst.
Path 5: QA and compliance leadership (preventing site failure)
If you are the person who notices risk before it becomes a finding, QA fits you. QA is where you turn “site stress” into documented control. Anchor your direction in the QA Specialist roadmap.
How to choose the right path in one question
Ask yourself: “What do I do naturally that reduces chaos for other people?”
If it is documentation and control, go regulatory or QA.
If it is systems and evidence, go data.
If it is stakeholder control and timelines, go PM.
If it is sponsor-facing oversight, go CRA.
Then reinforce your plan with salary context from the Clinical Research Salary Report 2025 and long-term earning trajectories from the top highest-paying clinical research jobs list.
6) FAQs: Clinical Trials Coordinator Career Path (2025)
-
Most sites use the titles interchangeably, but “Clinical Trials Coordinator” often emphasizes trial execution, visits, and protocol operations, while “Clinical Research Coordinator” may include broader study administration. In practice, what matters is your scope: do you run visits, manage consent and source, handle EDC queries, and own recruitment processes. If you want the cleanest salary context, use CCRPS benchmarking through the CRC Salary Guide 2025 and compare broader market anchors from the Clinical Research Salary Report 2025.
-
You win by proving you understand the site’s real pain: compliance risk, scheduling chaos, and data quality. Build a resume around transferable evidence work: documentation accuracy, process control, patient-facing communication, and time-critical operations. Then speak the language of trials: protocol navigation, consent discipline, source quality, and escalation habits. Add structured exam preparation using test-taking strategies and a focused study environment so you present as serious, not curious.
-
The fastest path is to own a measurable lane that impacts revenue or risk. Recruitment and retention performance is high leverage, especially when you can reduce screen failures and no-shows. Data quality is the other fast lever: reduce query aging, improve source-to-eCRF accuracy, and prevent repeat deviations through systems. Then you negotiate with proof and market context from the CRC Salary Guide 2025 plus broader comp trends in the Salary Report 2025.
-
Stop relying on memory. Build retrieval-ready documentation. Every key action should have a clear source trail: consent steps, visit procedures, lab handling, IP accountability, deviations and CAPAs, delegation clarity, and version control. Monitoring day should feel like demonstrating a system, not defending a scramble. If you want to formalize that mindset, study QA thinking through the QA Specialist roadmap and data discipline via the Clinical Data Manager roadmap.
-
It depends on what you can become exceptional at. CRA favors sponsor-facing oversight and cross-site operational discipline, supported by knowledge of systems like those in the remote monitoring tools guide. Regulatory rewards documentation power and approvals, mapped in the Regulatory Affairs Specialist roadmap. Data rewards evidence cleanliness aligned to the EDC platforms guide. PM rewards timelines and stakeholder control using salary context from the Project Manager salary trends guide.
-
Many people can reach senior or lead levels within 18 to 36 months if they stop being “helpful” and start being measurable. The timeline accelerates when you run complex protocols, improve recruitment conversion, or lead training and systems that reduce deviations and queries. If you stay in low-volume sites with weak infrastructure, growth can stall for years. That is why targeting strong environments from the academic medical centers list can be a career accelerator