How to Become a Clinical Research Coordinator (CRC): Your Step-by-Step Guide (2025)
Most people chasing a CRC role are not lacking intelligence. They are lacking proof of readiness. Hiring teams want to see you can protect patients, follow protocol, keep documents clean, and stay calm when a site is under pressure. This guide gives you a step-by-step path to become a Clinical Research Coordinator in 2025, plus the exact skills, credibility signals, and career moves that help you get hired faster and grow into higher-paying roles.
You will also see the salary levers, the common traps that delay offers, and the systems that make you look “site-ready” even if you are new.
1) What a Clinical Research Coordinator Does in 2025 (And What Hiring Managers Actually Want)
A Clinical Research Coordinator runs study execution at the site level. That means you translate protocol into real patient visits, protect informed consent, keep data and source documentation clean, and coordinate with monitors, sponsors, and vendors. The CRC is not a helper. The CRC is a control point. When a study is going well, a strong coordinator is usually the reason.
Hiring managers look for three signals: risk awareness, documentation discipline, and calm execution. They want someone who understands why compliance matters, not someone who memorized buzzwords. If you are coming from an entry path like a Clinical Trial Assistant or a Clinical Research Assistant, your advantage is task familiarity. Your challenge is proving you can own a workflow without constant supervision.
CRC work sits close to many other tracks, and understanding those tracks makes you more credible in interviews. If you can speak the language of data, you sound more senior, so review the Clinical Data Coordinator path and the Clinical Data Manager roadmap. If you can speak the language of quality, you sound safer to hire, so use the QA Specialist roadmap. If you understand regulatory expectations, you avoid rookie mistakes, so study the Regulatory Affairs Specialist guide and the Clinical Regulatory Specialist pathway.
The painful part most candidates do not realize: sites do not reject you because you are not smart. They reject you because onboarding a weak CRC is expensive. A weak CRC creates missing documents, late data, preventable deviations, and constant back-and-forth with monitors. The site pays for that with stress, reputational damage, and audits that become harder.
Your goal is to show you reduce stress, not increase it. That is the difference between “maybe” and “hired.”
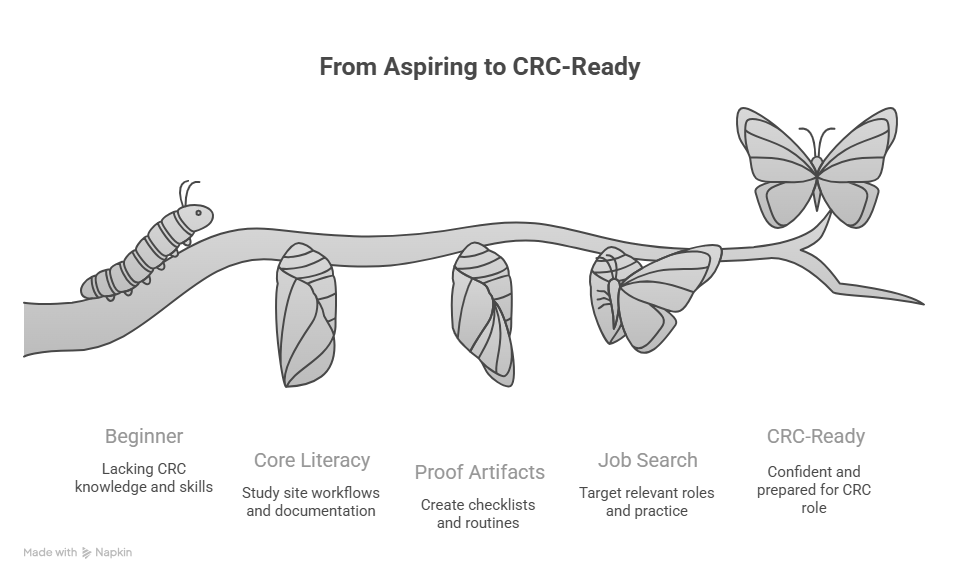
2) Step-by-Step: How to Become a Clinical Research Coordinator (CRC) in 2025
This path works whether you are new, switching from healthcare, or moving up from assistant roles. The key is building proof in the order hiring teams trust.
Step 1: Learn the site workflow before you chase titles
If you are starting from zero, do not jump straight to “CRC” as a label. Build workflow familiarity through roles that expose you to study operations, such as a Clinical Trial Assistant role or a Clinical Research Assistant path. The purpose is simple: you learn how studies actually run, how documents flow, and where mistakes get punished.
If you already have patient-facing experience, your edge is communication and patient trust. Your gap is research documentation discipline. Close that gap by learning what quality teams care about through the QA Specialist career roadmap and what regulatory teams care about through the Regulatory Affairs Associate guide.
Step 2: Build a CRC-ready skill stack that matches real site pain
Sites hire for pain relief. Your “skills” should map to site pain points:
Prevent consent errors
Keep visit windows under control
Keep source notes audit-ready
Close queries quickly and correctly
Keep essential documents organized
Coordinate PI and staff without confusion
If you want a high-value way to stand out, learn how sites are measured in modern trial ecosystems. Understanding platforms and workflows helps, even if you are not a data specialist. Review the Top 100 EDC and clinical data platforms directory and the Lead Clinical Data Analyst guide.
Step 3: Create “proof artifacts” that make you hireable faster
If you want offers, stop relying on a resume alone. Build proof artifacts you can describe in interviews:
A personal checklist for consent and version control
A visit scheduling system that protects window compliance
A query management routine that prevents repeat themes
A monitoring visit readiness checklist
A weekly mini-audit routine for essential documents
These artifacts make you sound like a safe hire because you think like someone who prevents problems. If you need structure for building disciplined routines, use CCRPS guidance on creating a strong study environment and proven test-taking strategies. The discipline transfers directly into how you work on a site.
Step 4: Get experience around investigators and delegation culture
CRC work is tied to investigator oversight. The more you understand PI responsibilities, the more useful you become. Review the Principal Investigator career roadmap and the Sub-Investigator pathway. You do not need to become a PI. You need to understand what they are accountable for so you can protect them.
Step 5: Choose the site environment that accelerates learning
Some sites train coordinators better than others. Academic medical centers often have deeper infrastructure and more active trials. If you are selecting where to apply, study the ecosystem using the Top academic medical centers with active trials list. Even if you do not apply to those exact sites, it helps you understand what “high-performing research culture” looks like.
3) The CRC Skill System That Makes You Look Experienced (Even If You Are New)
A CRC’s job is not “do tasks.” It is run a controlled process. The fastest way to look senior is to operate with systems.
System 1: Consent control system
Consent is the biggest risk zone for new coordinators. You need a simple system: verify the correct version, confirm all required signatures and dates, document the process, and store correctly. If you cannot explain your consent workflow confidently, you will not be trusted. Tie this back to quality thinking using the QA Specialist roadmap and regulatory thinking using the Clinical Regulatory Specialist pathway.
System 2: Visit window protection system
Most protocol deviations are not dramatic. They are quiet, preventable timing failures. A strong CRC builds a scheduling routine that respects windows, reminders, backup slots, and lab timing. This is how you protect data integrity and keep monitors calm. If you want to understand how data teams experience site performance, review the Clinical Data Manager roadmap and the Lead Clinical Data Analyst guide.
System 3: Query and data cleanliness system
Query volume is not always a sign you are doing badly. Query aging is. Sites get a reputation when queries sit untouched. Your system should include daily quick checks, weekly deeper cleanups, and root-cause prevention. If you can mention the modern data ecosystem intelligently, you sound more credible, so use the Top 100 EDC platforms directory to build vocabulary.
System 4: Monitoring readiness system
CRAs remember sites that are always ready. That translates into smoother visits, fewer follow-ups, and less stress. Build a monitoring readiness checklist and stick to it. If you want context on how monitoring has evolved, review the Top remote clinical trial monitoring tools guide. It helps you understand how sites are assessed even when monitors are remote.
System 5: Inspection readiness mindset
If your site gets audited, the audit is not “a bad day.” It is a test of daily discipline. A strong CRC runs small self-audits weekly and fixes issues early. Connect your mindset to quality leadership through the QA Specialist roadmap and to documentation expectations through the Regulatory Affairs Specialist guide.
4) How to Land Your First CRC Job (Resume Positioning, Interviews, and a 30-Day Plan)
If you want your first CRC offer, you must present as low risk. That means your resume and interview answers must show you understand compliance, site workflows, and documentation discipline.
Resume positioning that gets callbacks
Your resume should be built around controlled workflows, not generic duties. Replace vague lines with proof language:
Built scheduling workflows to protect protocol windows and reduce missed visits
Maintained regulatory and essential documents with version control discipline
Resolved data queries quickly and prevented repeat causes through process fixes
Supported monitoring readiness with structured document staging and follow-up
If you need guidance on how clinical careers are structured, use role roadmaps like the Clinical Research Administrator pathway and salary context like the Clinical Research Salary Report 2025. Those resources help you sound aligned with how the industry thinks.
Interview answers that make you sound site-ready
CRC interviews are rarely about theory. They are about scenarios. Expect questions like:
How do you prevent consent errors
How do you handle a missed visit window
How do you respond to an urgent safety event
How do you prepare for a monitoring visit
How do you manage data queries and source notes
To strengthen your interview discipline and preparation structure, use CCRPS resources like proven test-taking strategies and building the perfect study environment. The routines they teach will help you prepare like a professional, not like a nervous beginner.
A practical 30-day plan to become “CRC-ready” fast
Days 1 to 10: Build core site workflow literacy
Study consent steps, version control, and visit schedule logic
Learn how essential documents are organized
Practice writing clean, audit-ready notes
Days 11 to 20: Build your proof artifacts
Create a consent checklist and a visit window checklist
Create a monitoring readiness checklist
Create a query management routine
Days 21 to 30: Build your job search strategy
Apply to sites with active trials and strong infrastructure
Target roles that touch research workflows, not unrelated admin tasks
Prepare scenario answers and practice calm communication
If your long-term goal is to move beyond CRC, map out the ladder using adjacent CCRPS career guides such as the CRA salary and role landscape and the Clinical Trial Manager salary and operations context.
5) CRC Salary Guide 2025 (What Affects Pay and How to Grow Fast)
CRC pay varies by site type, study complexity, location, and how much responsibility you actually carry. The biggest mistake is negotiating without understanding how clinical organizations price risk.
Start with market context using the Clinical Research Salary Report 2025 and the CRC salary guide for 2025. Then compare how salary scales as you move up the ladder using the Top 10 highest paying clinical research jobs and the CRA salary report.
The levers that raise CRC compensation
Scope: If you coordinate more studies, more patients, or more complex protocols, pay rises.
Complexity: Oncology, rare disease, device trials, and complex endpoints usually pay higher because execution risk is higher.
Quality performance: Sites value CRCs who prevent deviations and maintain inspection readiness.
Speed and reliability: Coordinators who keep data and documents moving reduce monitoring friction and sponsor escalations.
If you want to move into specialized tracks that often raise compensation, learn the landscape through the GCP certified professional salaries guide and consider how data-heavy roles scale using the Clinical Data Manager roadmap.
How to negotiate without sounding unrealistic
Negotiate based on scope and value. Ask what you will own, how many studies you will support, what systems exist, and what “good performance” looks like. Then anchor your request to market references like the CRC salary guide 2025 and the broader salary report.
Also, understand your next step. Many CRCs move into CRA, CTM, regulatory, data, or QA. Your salary growth accelerates when you choose a track and build proof. Use the Regulatory Affairs Specialist roadmap, the QA Specialist roadmap, and the Clinical Data Coordinator path to see how those ladders work.
6) FAQs: Becoming a Clinical Research Coordinator (CRC) in 2025
-
Yes, but you must reduce perceived risk. Sites fear onboarding someone who creates compliance problems. Build proof artifacts like a consent checklist, visit window system, monitoring readiness routine, and documentation habits you can explain clearly. Start in roles that expose you to workflows such as a Clinical Trial Assistant or a Clinical Research Assistant, then move into CRC when you can demonstrate controlled execution.
-
Informed consent discipline is the highest-impact skill because errors carry serious consequences. Master version control, documentation clarity, and patient-centered communication. Then build visit window control, because timing failures create deviations and data gaps. Strengthen your quality mindset using the QA Specialist roadmap and your regulatory awareness using the Clinical Regulatory Specialist pathway.
-
Prepare scenario answers, not definitions. Practice how you prevent consent errors, handle missed windows, respond to safety urgency, prepare for monitoring visits, and resolve queries. Use structured preparation habits from proven test-taking strategies and consistency routines from building the perfect study environment.
-
Expectations depend on location, site type, and complexity. Use the CRC salary guide 2025 and the Clinical Research Salary Report 2025 to benchmark. If you want to understand your upside as you grow, compare to the CRA salary report and the highest paying roles list.
-
CRCs who become CRAs faster usually excel in monitoring readiness, query resolution, and deviation prevention. They understand protocol deeply, keep documentation clean, and communicate clearly with monitors. Use the CRA salary and market report to understand the role’s expectations and how companies evaluate readiness.
-
Common paths include CRA, Clinical Trial Manager, Clinical Operations Manager, Regulatory Affairs, Quality Assurance, and Clinical Data roles. Explore the ladders using the QA Specialist roadmap, the Regulatory Affairs Specialist roadmap, and the data paths like the Clinical Data Manager guide.
-
They try to “work harder” instead of building systems. CRC work is endless if you do not control it. The fastest way to succeed is to build routines for consent, visit windows, queries, monitoring readiness, and document checks. Those routines reduce stress and protect compliance. If you need a discipline framework, use the structure in creating the perfect study environment and proven test-taking strategies because they teach consistent execution under pressure.