Clinical Research Project Manager Career Path Comprehensive Guide
Clinical Research Project Managers are the people sponsors trust when timelines slip, sites underperform, and budgets start bleeding. If you want this career path, you need more than “project management.” You need clinical operations fluency, risk-first thinking, and the ability to turn chaos into execution without burning teams out. This guide breaks down exactly what you own, how to move into the role step by step, what skills actually get you hired, and how to prove you can run trials end to end using real outputs and measurable wins.
1) What a Clinical Research Project Manager Actually Owns (And Why Teams Respect Them)
A Clinical Research Project Manager (CRPM) is not a meeting scheduler. You are the owner of trial execution outcomes, which means you live where operational risk meets compliance. The fastest way to understand the role is to think in “deliverables, dependencies, and decisions.” You translate protocol intent into a working plan across sites, vendors, and internal functions, using the same execution discipline you see in high-performing clinical operations teams. If you are coming from roles like Clinical Trial Assistant (CTA), Clinical Research Assistant, or Clinical Research Administrator, your edge is that you already understand the trial engine. Now you must learn how to run it with accountability.
CRPMs typically own the integrated timeline, the study budget tracking, the risk register, and the decision cadence across stakeholders. You are also the person who sees the full system: enrollment velocity, screen fail rate, query aging, vendor turnaround, safety reporting flow, and site performance trends. If you have worked alongside monitoring teams, use the lens of CRA compensation and scope to understand where monitoring effort expands and where your coordination must tighten. If you are closer to data, you still need to know how DM decisions ripple into timelines, similar to what a Clinical Data Manager or Clinical Data Coordinator fights daily.
Your credibility is built on preventing avoidable pain: missed milestones, uncontrolled change requests, unclear responsibilities, and weak communication that creates rework. Sponsors pay for predictability. Sites want clarity. Vendors want clean requirements. Your job is to make all three true at the same time while protecting quality. That is why CRPMs who understand compliance and documentation standards move faster and get trusted sooner, especially when they can speak to GCP realities and compensation signals like those reflected in GCP-certified professional salary trends and broader clinical research salary benchmarks.
2) Career Ladder to Clinical Research Project Manager: Step-by-Step Roadmap That Actually Works
If you want to become a CRPM, stop chasing titles and start chasing ownership. Hiring managers promote the person who can take a messy workstream, stabilize it, and prove impact with metrics. That is the same reason certain feeder roles accelerate faster, especially roles with exposure to cross-functional coordination such as Clinical Research Assistant, Clinical Trial Assistant (CTA), and Clinical Research Administrator. Your goal is to move from “task doer” to “outcome owner” without pretending you already are a PM.
Step 1: Pick a workstream you can own end to end. That could be site activation readiness, vendor issue resolution, recruitment tracking, or query aging reduction. If your background is data-heavy, anchor your credibility by understanding what senior data roles demand, similar to the path described in the Lead Clinical Data Analyst career guide and the operational dependencies outlined in the Clinical Data Manager roadmap. If your background is regulatory, you can build a promotion narrative through site and submission coordination using the frameworks found in the Regulatory Affairs Specialist roadmap and the adjacent Clinical Regulatory Specialist pathway.
Step 2: Convert your work into a PM artifact. A CRPM is judged by the tools they build and maintain: a risk log, a decision log, a milestone tracker, a vendor escalation path, and a weekly status summary that forces decisions. Use the discipline in proven test-taking strategies as a mindset model: you win by controlling variables, not by hoping things work out. If you cannot create a clean “one-page” status, you are not ready to run a trial.
Step 3: Learn the language of risk and escalation. Many smart candidates fail here because they either escalate too late or escalate emotionally. A CRPM escalates with options, consequences, and a decision ask. You can sharpen this skill by studying how high-risk functions operate, like pharmacovigilance coordination in a Drug Safety Specialist career progression or leadership responsibilities in a Pharmacovigilance Manager roadmap. You are not switching careers into PV, you are borrowing the mindset of early warnings and controlled workflows.
Step 4: Become fluent in cross-functional incentives. Sites want feasibility support and predictable processes. Data teams want clean inputs and fewer late changes. Monitors want stable plans that match reality on the ground, which is why reading salary and scope breakdowns like the CRA salary report and the Clinical Research Coordinator salary guide is useful. It teaches you what each function values and why.
Step 5: Target the “Assistant PM” or “Project Specialist” bridge role. If your organization does not have a formal bridge, manufacture one by taking on PM tasks that nobody wants: meeting cadences, metric reporting, vendor follow-ups, and change request tracking. Your internal pitch becomes credible when you can say, “Here is the baseline, here is the risk profile, here is what changed, and here is the measurable improvement.” When you can do that, you are already functioning like a PM, even if your title has not caught up.
3) Skill Stack That Gets You Hired: Tools, Metrics, and Leadership That Separate You From the Crowd
Most candidates try to “learn project management.” That is too generic. Clinical research PM hiring is about whether you can manage trial complexity without hiding behind buzzwords. Your skill stack must be practical, measurable, and tied to trial delivery, similar to how specialized roles build targeted mastery in guides like the Clinical Medical Advisor pathway or the Medical Science Liaison roadmap. Again, you are not pivoting into those roles, you are learning how cross-functional leaders think.
1) Planning you can execute, not planning you can present. A PM plan fails when it is too complicated to run weekly. Your plan should include: critical path, milestones, owners, dependencies, escalation triggers, and buffer logic. If you struggle with consistency, build your routine the same way you would build a study routine using the perfect certification study environment. Execution requires a system, not motivation.
2) Metrics that expose problems early. A CRPM who only reports “green status” is a liability. You need a small set of metrics that reveal drift before failure happens. Examples: enrollment against forecast, screen fail patterns by site, query aging bands, monitoring visit backlog, vendor turnaround time, and protocol deviation categories. Tie your understanding of market expectations to compensation and role demand by referencing career pay context like the Clinical Research salary report and the role value signals in Project Manager salary trends. These resources help you see which skills are being rewarded right now.
3) Vendor management discipline. Many new PMs get crushed here because they treat vendors like teammates instead of contracted performance partners. You need clear acceptance criteria, response SLAs, and a written escalation ladder. If you have never managed vendors, learn by studying vendor ecosystems and tooling lists such as the Top 50 contract research vendors and platforms and the Top 50 remote clinical trial monitoring tools. Your advantage in interviews is being able to explain how tools fit into workflow and risk control, not listing tool names.
4) Recruitment realism and feasibility skepticism. Enrollment is where timelines die. You need to understand feasibility inputs, recruitment assumptions, and what patient recruitment partners can and cannot do. Even if you are not buying services today, you should know what the market looks like by scanning resources like the Top 75 patient recruitment companies and solutions and how top institutions run active research pipelines via the Top academic medical centers list. This makes you more credible when you talk about feasibility and site strategy.
5) Leadership that reduces friction. A CRPM does not “manage people” in the traditional sense, but you lead through clarity, calm escalation, and decisions. Your leadership is visible in the quality of your agendas, your action items, your stakeholder updates, and your ability to remove blockers. If you cannot lead a meeting to a decision, you will drown in meetings forever. That is the difference between busy and effective.
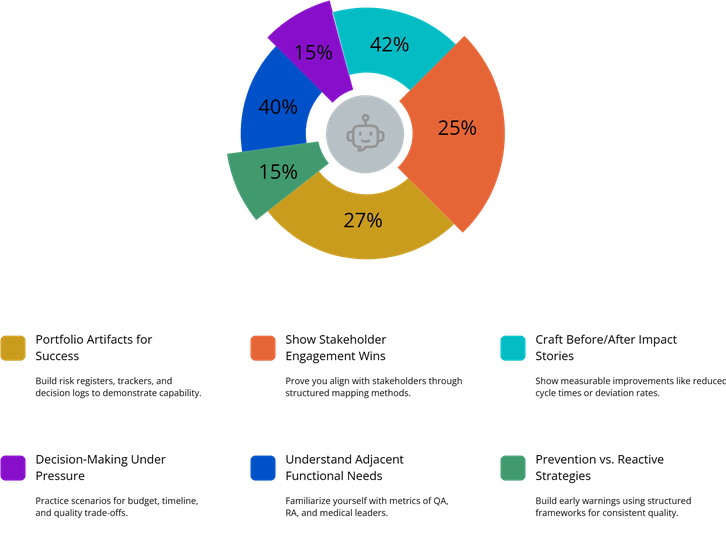
4) How to Build Credibility Fast: Portfolio Proof, Stakeholder Wins, and Interview Stories
Clinical research PM interviews are not won by saying you are “organized.” They are won by showing how you think when trials go sideways. You need proof that you can make decisions with imperfect information, keep quality intact, and still move execution forward. Your credibility comes from artifacts and outcomes, the same way credibility is established in specialized career roadmaps like the Sub-Investigator pathway or the Principal Investigator roadmap, where responsibility is measured by what you own, not what you claim.
Build a portfolio that looks like you already do the job. You do not need confidential documents. You need realistic templates: a milestone tracker, a risk register with escalation triggers, a weekly status format, and a decision log. Add a stakeholder map that shows who you align with and why. Create a vendor performance tracker that includes turnaround, quality errors, and escalation thresholds. If you can build these cleanly, you will stand out against candidates who only list skills.
Create “before and after” stories with numbers. For example: you reduced query aging, improved site activation cycle time, stabilized enrollment forecasting, or lowered deviation frequency by tightening training and communication. If you come from monitoring, you can anchor your story in operational realities you see in CRA life, which you can frame using market context like the CRA salary report and the ecosystem of remote monitoring tooling shown in the remote monitoring tools guide. If you come from data, tie your story to data workflow stabilization using the EDC platforms mega list.
Prove you can handle cross-functional tension. A CRPM is often the person who must say, “We can’t do all of that by that date with this budget.” That requires calm confidence and a structured decision process. Practice framing tradeoffs: what happens if enrollment slips two months, what cost increases follow, what quality risks rise, and what mitigation options exist. If you can do this clearly, you sound like leadership. If you cannot, you sound like a coordinator.
Interview answers must show prevention, not just recovery. Anyone can “work hard” when things break. High-value PMs prevent predictable failures by building early warning systems. Use the same structured mindset you would use in exam performance frameworks from test-taking strategies. The best PMs are not the loudest. They are the clearest.
Your final credibility accelerator is learning how other functions measure success. Read adjacent career guides, not to switch roles, but to understand incentives: Quality Assurance Specialist career expectations, Regulatory Affairs Associate work scope, and Clinical Medical Advisor cross-functional leadership. When you can speak to the pressures each function faces, your communication becomes more effective and your leadership becomes more believable.
5) Salary, Locations, and Negotiation: What Actually Moves Your Offer in 2025
CRPM compensation is not only about years of experience. It is about the complexity you can handle without supervision. Two candidates with the same time in industry can land very different offers if one can run budgets, vendors, and risk escalations cleanly. Anchor your expectations with market context from the Clinical Research Project Manager salary trends guide and compare it to broader role benchmarks in the Clinical Research salary report. Those references help you understand what “normal” looks like and when you have leverage.
What raises offers fastest: ownership of multiple studies, sponsor-facing leadership, vendor oversight, and a track record of hitting milestones with quality intact. If you have experience in high-demand adjacent areas, you often move up faster. Examples include decentralized components and remote monitoring coordination, which you can connect to the market tooling landscape in the remote monitoring platforms guide, or recruitment execution understanding informed by the patient recruitment companies list.
Location still matters, but leverage is shifting. Hybrid and remote structures are common in CRO and sponsor ecosystems, but the highest trust roles often require strong stakeholder presence, at least periodically. Use the salary context from related roles to calibrate your negotiation narrative: the CRA salary report, the Clinical Research Coordinator salary guide, and the Top 10 highest-paying clinical research jobs list. This helps you frame why your skill stack deserves the top of band.
Negotiation is easier when you bring outcomes, not opinions. Instead of “I deserve more,” say: “I have owned vendor escalations, stabilized milestone reporting, reduced cycle time, and improved predictability.” Then tie it to risk reduction: “That prevents budget surprises and protects quality.” Sponsors pay for fewer unpleasant surprises.
One more advantage most candidates ignore: your ability to communicate clearly. A CRPM with executive-ready writing is rare. If your weekly status updates can be read in two minutes with decisions obvious, you become indispensable. Create that skill the same way you create a high-performing routine using the right study environment principles. Consistency creates results.
6) FAQs(Frequently Asked Questions)
-
The fastest path is to own a cross-functional workstream and convert it into PM-style artifacts. Start in roles with coordination exposure like Clinical Trial Assistant (CTA) or Clinical Research Administrator, then take ownership of timelines, risk tracking, and stakeholder updates for a piece of the study. Build a portfolio template set: milestone tracker, risk log, decision log, and status report. In interviews, tell one story where you prevented a predictable failure through early warnings and escalation discipline. Hiring managers promote “outcome owners,” not task collectors.
-
You do not need it, but it helps because it builds trial intuition. CRA experience teaches execution realities and site constraints, which are reflected in scope differences seen in the CRA salary report. CRC experience builds enrollment and site workflow fluency, often tied to compensation patterns seen in the CRC salary guide. If you come from data or regulatory, you can still become a CRPM by proving you understand cross-functional dependencies using resources like the Clinical Data Manager roadmap or the Regulatory Affairs Specialist roadmap.
-
Learn tools that support decision-making and risk control, not vanity tools. Prioritize: milestone tracking, risk logs, issue logs, and simple KPI reporting. Then understand the ecosystem you coordinate, including monitoring and data platforms. Review the market landscape in the remote monitoring tools guide and the EDC platforms mega list so you can speak intelligently about workflows. Your goal is to explain how tools reduce cycle time, prevent deviations, and improve predictability.
-
You prove budget readiness by showing you understand cost drivers and change control. Build a mock budget tracker tied to milestones and vendor scope. Learn how change requests create cost expansion through monitoring intensity shifts, recruitment delays, and vendor add-ons. Then practice describing tradeoffs: what gets cut, what gets delayed, and what quality risks rise. Use market context from the Project Manager salary trends guide to understand why budget ownership increases compensation and trust. In interviews, explain one scenario where you prevented cost growth by tightening scope and escalation timing.
-
The most common failures are late escalation, weak decision asks, and status reporting that hides risk. New PMs often over-meet and under-decide. They also fail to align stakeholders early, so problems emerge as surprises instead of expected risks. Build escalation discipline using structured thinking similar to the frameworks in test-taking strategies, where you control variables and act early. A strong CRPM makes risk visible, proposes options, and forces a decision path before timelines collapse.
-
Bring artifacts and metrics. Show a one-page status report format, a risk log with triggers, and a stakeholder map. Then tell a prevention story with numbers: improved cycle time, reduced query aging, stabilized enrollment forecasting, or lowered deviations. Tie your understanding of the market to role value using the Clinical Research salary report and the Project Manager salary trends guide. Hiring managers want proof you can protect predictability under pressure.
-
Senior progression is driven by your ability to run multiple studies, manage vendors, protect budgets, and maintain sponsor trust. You must improve your forecasting, escalation, and executive communication. Learn the vendor ecosystem and how performance is measured using the Top CRO vendors and platforms guide. Understand recruitment realities through the patient recruitment solutions list. Senior leaders see systems, not tasks. Your job is to become a systems operator who reduces surprises.
-
Do not try to learn everything at once. Build a structured weekly system and stack skills in layers: first cadence and reporting, then risk and escalation, then vendor and budget discipline. Use routine-building guidance like creating the perfect study environment to design consistency. Add focused study using test-taking strategies so you improve faster with less wasted time. Overwhelm usually comes from unstructured learning. A CRPM mindset is structured execution.